Flip Chart
Use the 2-sided presentation tool to walk your patients through LSS, their treatment options, and what to expect with the mild® Procedure.
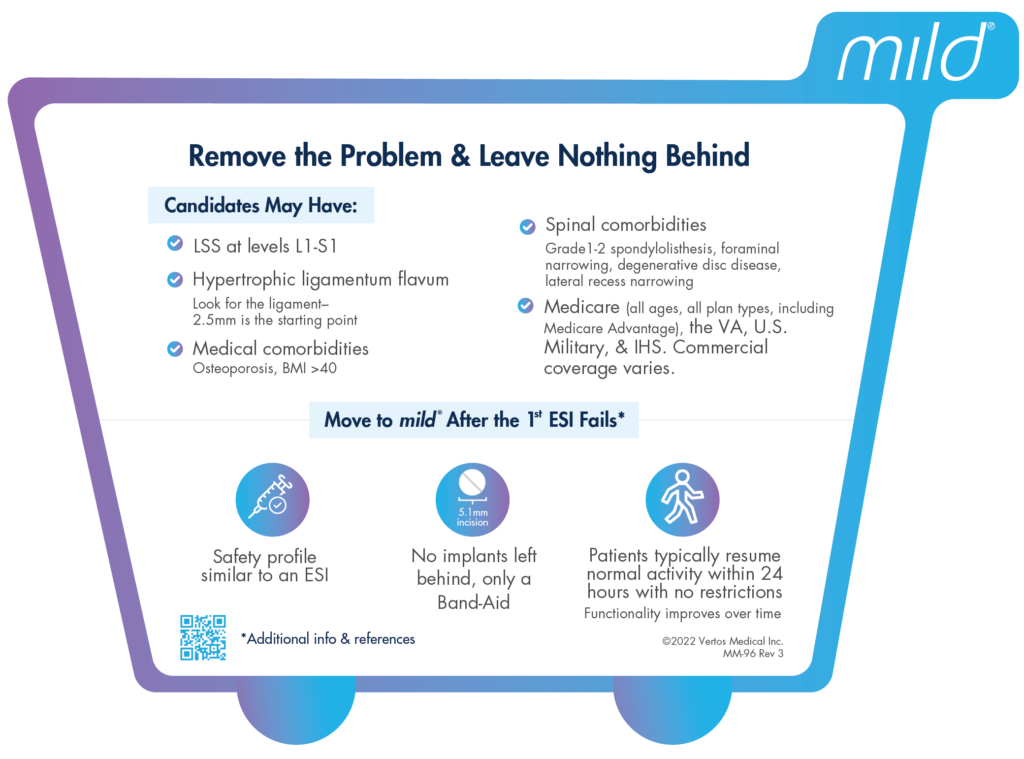
Many providers are moving beyond epidural steroid injections (ESIs) for patients with chronic low back pain associated with lumbar spinal stenosis (LSS).
Instead of simply masking the pain caused by an enlarged ligament with epidural injections, which may only provide temporary pain relief, providers now opt for more innovative and durable spinal stenosis treatment options such as the mild® Procedure.
An epidural steroid injection, which is a medication that is injected into the epidural space in the lower spine to reduce swelling and offer pain relief, may be offered to patients with chronic low back pain from conditions such as lumbar spinal stenosis.
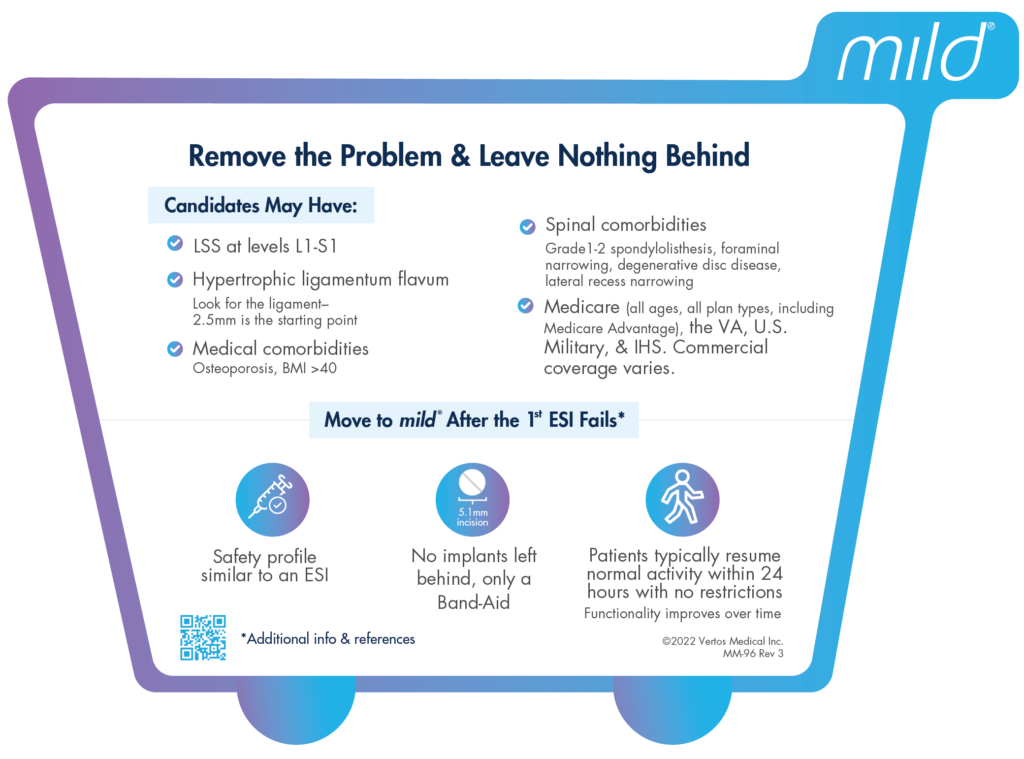
Recent data indicates that repeat epidural injections for patients who experience only short-term improvement may not be in the patient’s best interest in the long term. Alternative treatments, such as minimally invasive lumbar decompression, or the mild® Procedure, may be a better option for some patients.
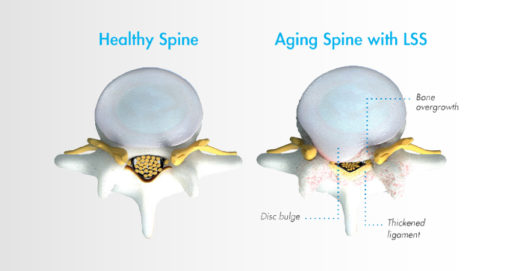
Lumbar spinal stenosis, also called LSS, contributes to chronic low back pain and is prevalent in approximately 20 percent of patients over the age of 60. LSS is often caused by an enlarged ligament in the back, which compresses the space around the spinal canal and puts pressure on the nerves in the lower back. This pressure around the spinal cord can cause pain, numbness, heaviness, or tingling in the low back, legs, and buttocks. A common visual cue is often referred to as the “shopping cart syndrome,” where the act of leaning over, often over a shopping cart, cane, or walker, helps to temporarily alleviate pressure felt in the lower back pain.
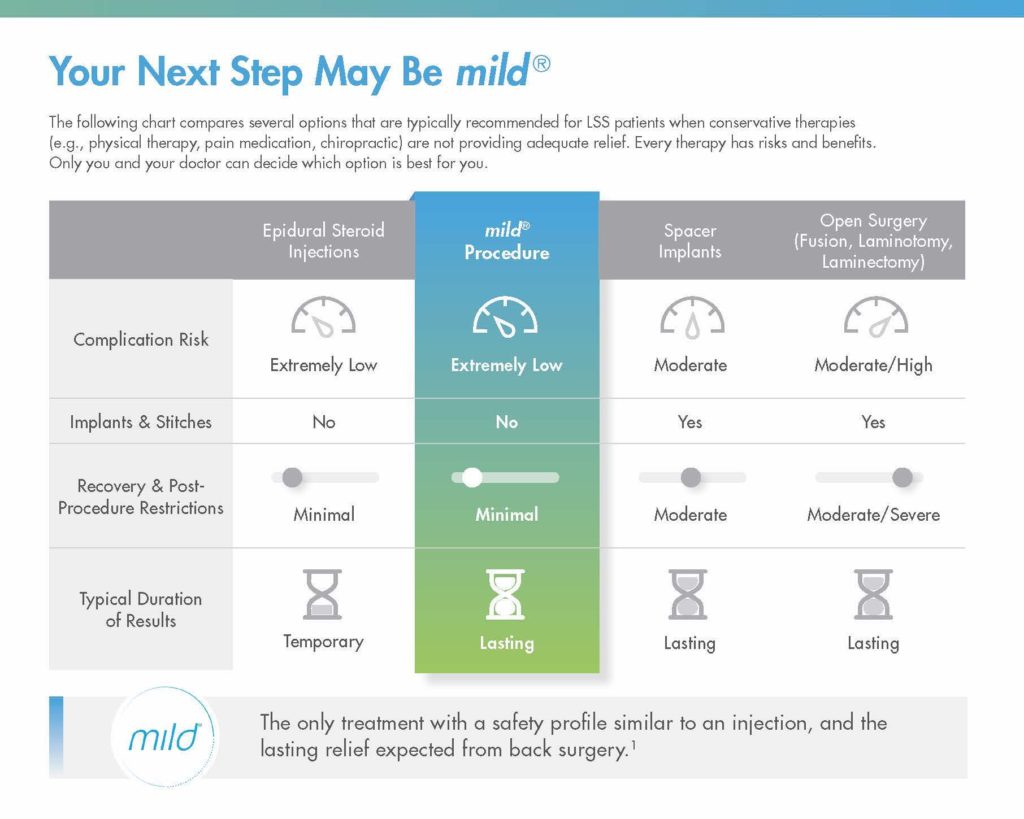
In addition to epidural steroid injections, some common conservative treatment options for LSS can include the mild® Procedure, medication, and/or physical therapy, with more invasive options including procedures such as spacer implants, spinal stenosis surgery, or other open surgery.
Epidural steroid injections are typically offered to LSS patients when more conservative treatment options, such as exercise and physical therapy, have failed to provide relief.
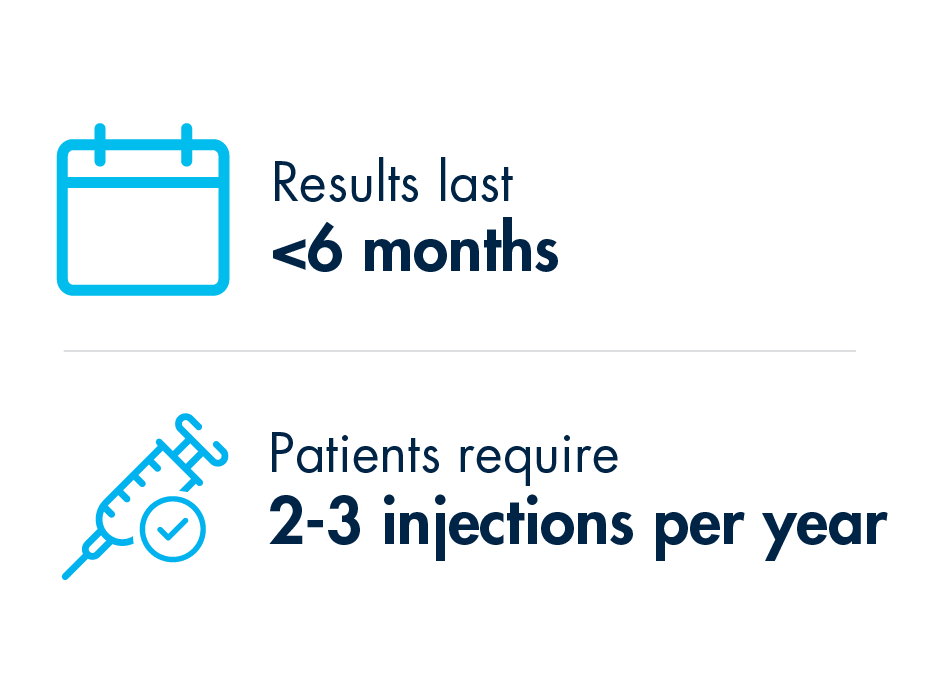
Steroid medication is injected directly into the epidural space, which may relieve pain by reducing inflammation around the spinal cord and nerves. The effects typically last for less than 6 months, after which additional injections may need to be administered.
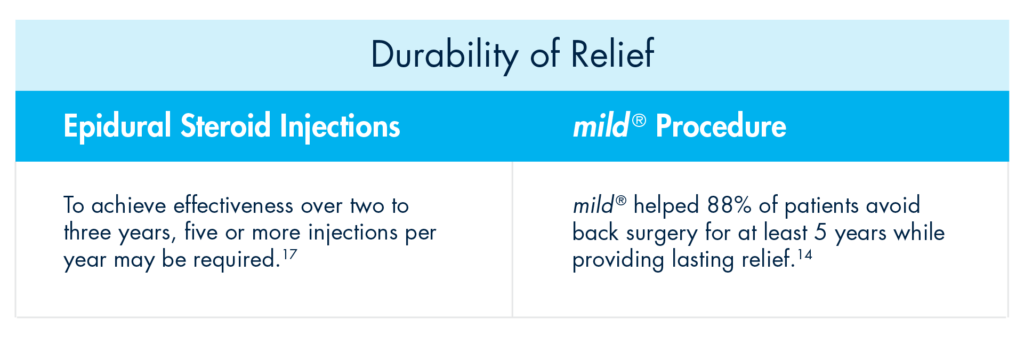
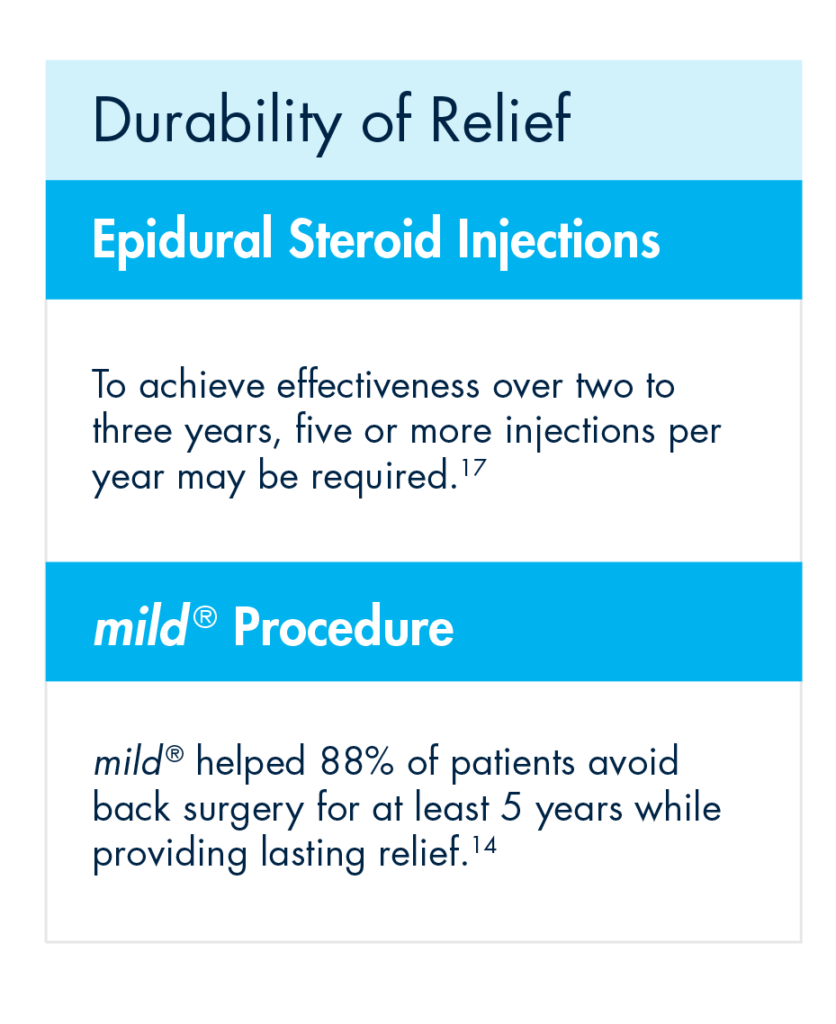
Data shows that epidural steroid injections can effectively relieve pain for LSS patients—but the effects are not lasting, and pain may return, typically in months. ESIs treat the symptoms but do not address the root cause of pain associated with LSS.
While ESIs are an effective form of early treatment for some patients, they may not provide reliable, lasting relief for all low back pain.
As mentioned in the Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST), certain payer guidelines, including Centers for Medicare and Medicaid Services (CMS), now stipulate that patients should have obtained a minimum of 3 months of pain relief with eventual recurrence of pain before it is reasonable to proceed with additional injection therapy.
This means that for patients exhibiting shorter-term relief of less than 3 months after receiving an ESI, clinicians should consider alternative treatment options.
Steroid medication reduces inflammation, which can temporarily relieve pain. However, epidural steroid injections only treat the symptoms of LSS—not the root causes of pain and inflammation. The effects of epidural steroid injections typically last less than 6 months, and patients often require an average of 2–3 injections per year to sustain long-term relief from low back pain associated with LSS.
There are many patients for whom repeat epidural steroid injections may offer more risks than benefits. For instance, steroid medications have been linked to bone loss, or osteoporosis. ESIs may also introduce risks for patients with certain comorbidities such as diabetes, cardiovascular conditions, active infections, bleeding disorders, or those taking anticoagulant medications.
As an alternative, epidural injections without the use of steroids may be considered, as well as more advanced decompressive therapies such as the mild® Procedure.
In addition to the health concerns associated with repeat steroid injections, the mental and emotional effects experienced by many LSS patients can also reveal the dark side of repeat epidural steroid injection treatments.
Due to the temporary nature of epidural steroid injection relief and the requirement for repeat injections, many practices encounter patients with what is increasingly becoming known as “ESI Exhaustion.” ESI Exhaustion can be spotted in patients at any stage of LSS treatment or stenosis severity.
When patients experience short-term relief for a condition as challenging as LSS, they can easily become frustrated and lose hope. LSS patients often experience debilitating pain and loss of mobility that can have a devastating impact on their outlook and optimism for the future. Losing additional time and energy to repeated appointments, procedures, and recovery times can also be detrimental to their quality of life, and some patients may start to feel hopeless if injections remain ineffective or lose their efficacy soon after receiving them.
One of the more common questions patients have about a steroid injection is, “How long will the results last?” Unfortunately, with epidural steroid injections, efficacy can vary by patient, and it can be difficult to predict the degree of relief or durability of effect for the individual. While studies have shown symptom relief for up to 6 months in some lumbar spinal stenosis patients, other studies have demonstrated the limited effectiveness of epidural steroid injections.
If patients are dissatisfied with their results and feel they have run out of options in your practice, they may search for another solution. By offering alternative treatments such as the mild® Procedure as an early intervention, you can retain the patients in your practice and increase productivity, while continuing to develop closer relationships and increase your reach within your community.
Given the significant advances in minimally invasive spine technology, current research confirms that repeat epidural steroid injections should be reserved only for patients who experience significant and lasting relief after the injections, and/or those who are not candidates for higher-level interventions or surgical decompression.
For patients experiencing relief that lasts fewer than 3 months, clinicians may wish to consider more durable treatment options.
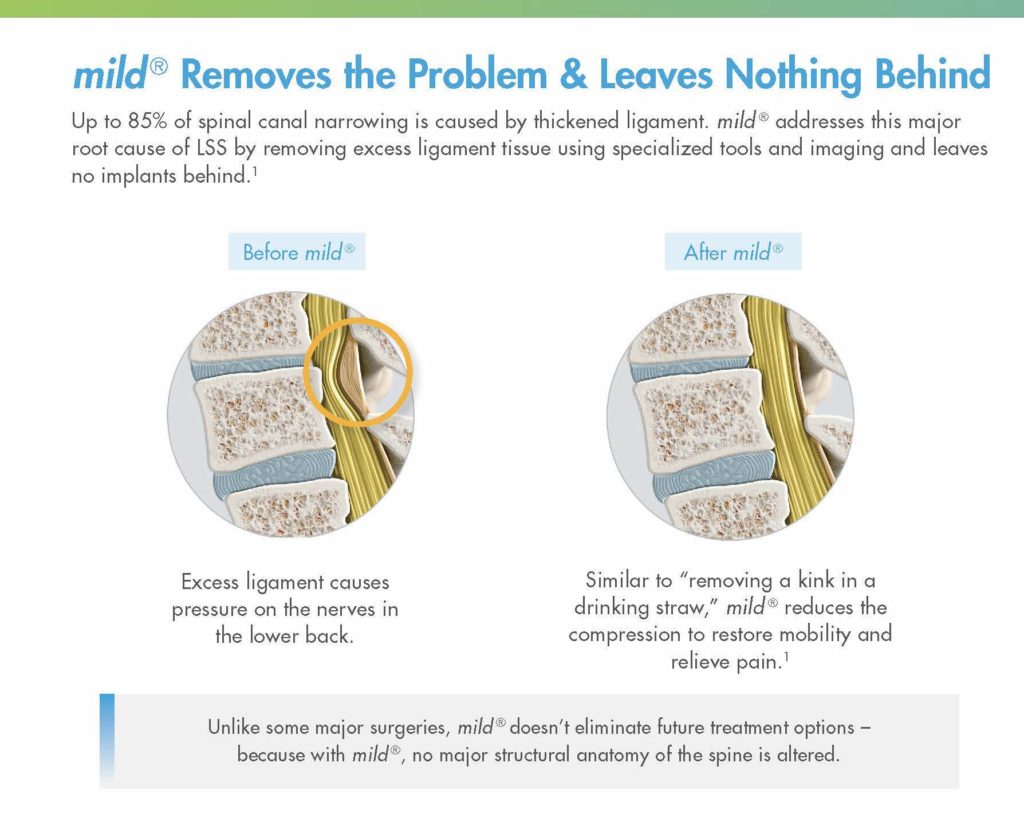
While they may offer temporary relief, epidural steroid injections do not “cure” LSS. Without addressing the enlarged ligament, which contributes up to 85% of spinal canal narrowing , relief may only be experienced on a short-term or temporary basis.
Minimally invasive lumbar decompression may be the next step for long-lasting relief from LSS and to reduce pressure in the canal. By decreasing the amount of space taken up by the enlarged ligament, patients can experience decreased pressure on the spinal nerves, which may lead to decreased pain.
Performing multiple epidural steroid injections only delays patients from receiving treatment with more lasting results, such as minimally invasive lumbar decompression—the mild® Procedure.
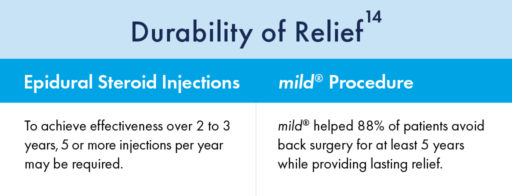
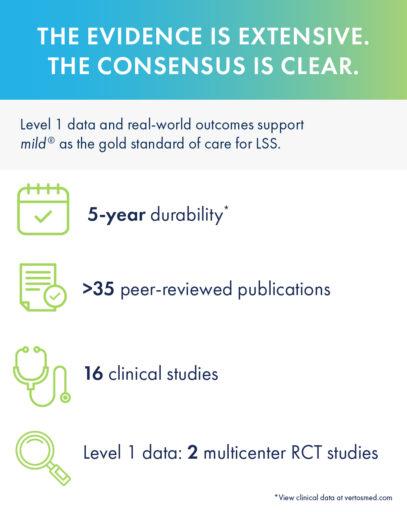
Turning to mild® as the first line of therapy addresses the root cause of LSS by removing excess ligament tissue around the spine, proven to provide a 5-year durability of results.
The mild® Procedure is a short, outpatient procedure that can be performed using only local anesthetic and light sedation. The procedure is performed through a single incision in the low back smaller than the size of a baby aspirin, or the diameter of a drinking straw (5.1mm).
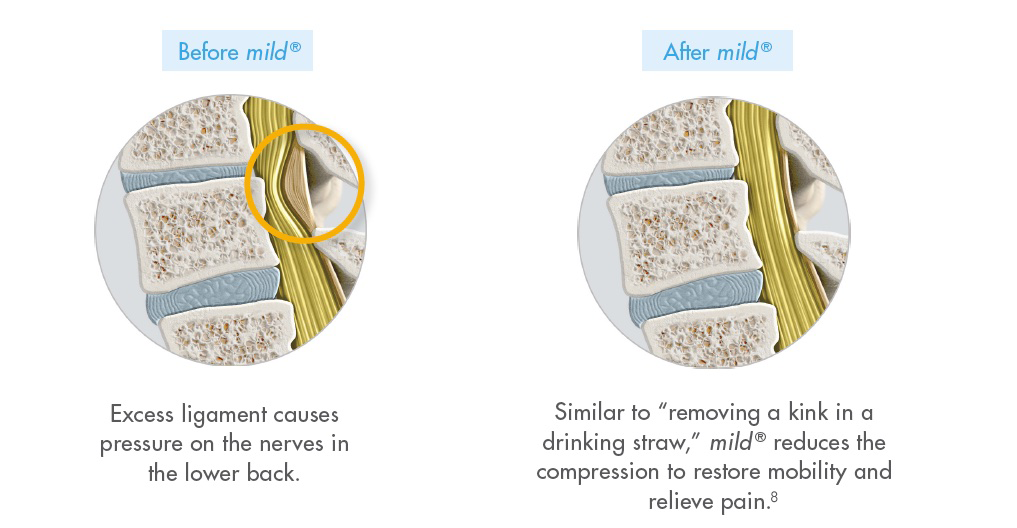
By removing excess ligament tissue that has built up around the spine, mild® restores space in the spinal canal. This reduces pressure on the nerves in the low back, addressing a major root cause of LSS, which can help reduce pain.

When Epidural Steroid Injections (ESIs) Don’t Provide Lasting Relief, mild® can improve patient outcomes across a variety of measures:
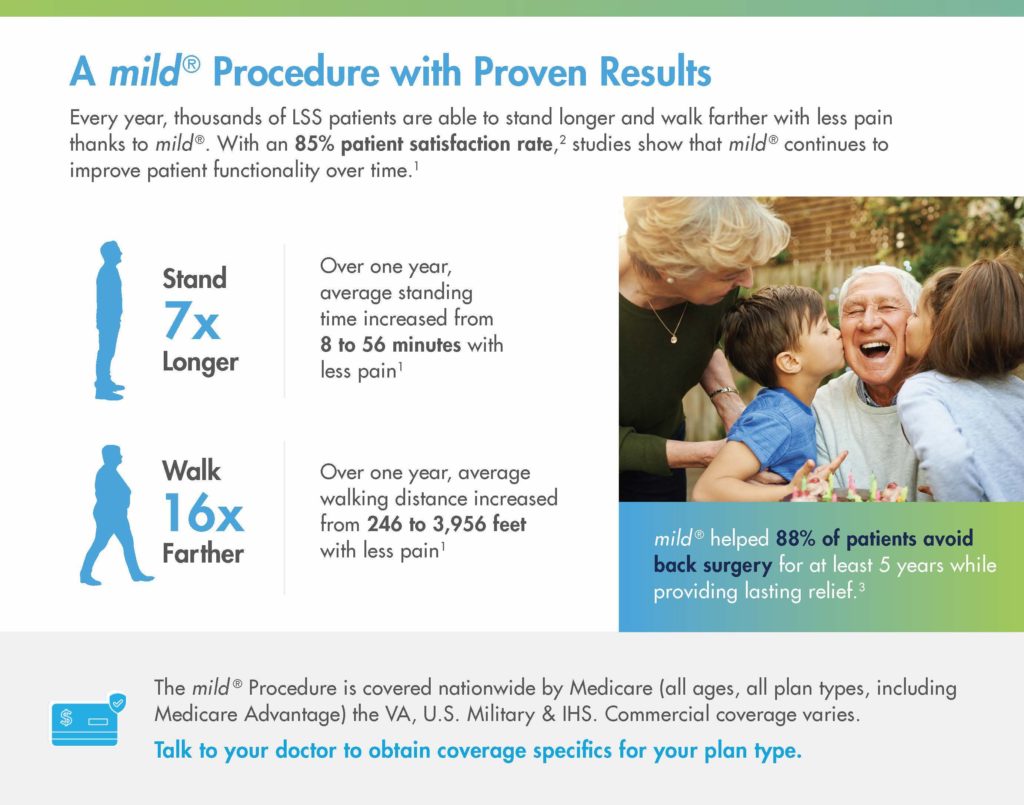
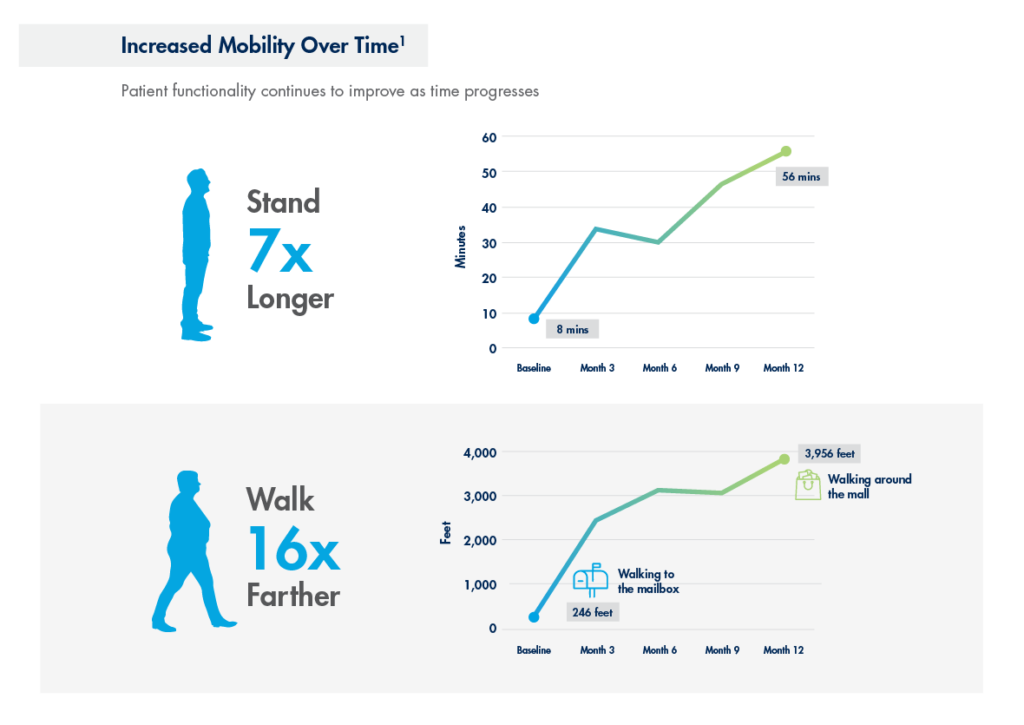
In a study performed at the Cleveland Clinic 1 year after the mild® Procedure, patients were able to:
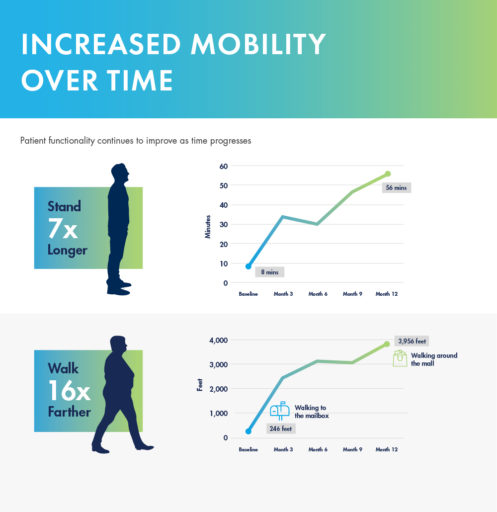
mild® demonstrated excellent long-term durability with significant improvements in both pain and mobility over 2 years. Clinical data from the MiDAS ENCORE 2-Year Study finds mild® provided patients with lasting pain relief and increased mobility.
A 5-year study performed at the Cleveland Clinic demonstrated that mild® helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief. Use our Find a mild® Doctor tool to connect with an interventional pain management specialist in your local area to find out if mild® is right for you.
To learn more about mild® and how it can help people suffering from LSS get on the path to lasting relief, explore mildprocedure.com.
In the evolving landscape of medical care, collaboration between different specialties is proving to be a game-changer for patients dealing with complex conditions. One such collaborative effort that stands out is the partnership between interventional pain physicians and spine surgeons in managing lumbar spinal stenosis (LSS). This contemporary approach aims to provide patients with a continuum of care that merges the expertise of both fields, resulting in better outcomes and improved patient experiences.
Historically, the divide between pain management and surgical intervention was palpable. However, this narrative is rapidly changing, as exemplified by the journey of Dr. Stevenson, a veteran neurosurgeon, and Dr. Antony, an interventional pain physician. Their collaboration, cautious at first, quickly evolved into a transformative model of patient care.
The key to this success lies in breaking down perceived barriers. Both specialists found that open communication, transparency, and a shared goal of patient well-being were the bridges that brought them together. Instead of focusing on the contrast between their specialties, they recognized the value of mutual learning. This synergy allowed for comprehensive discussions surrounding spinal stenosis treatment options. Topics of open discussion included MRI interpretations, indications for different procedures, and when surgery should be considered as an early option. It was a shift from a mindset of “last resort” to “best-suited solution.”
One of the most remarkable aspects of this collaboration was the way it empowered advanced practice providers (APPs), such as physician assistants (PAs), to become integral members of the patient care team. Armed with the ability to read imaging, understand evidence-based outcomes, and confidently make clinical decisions, APPs played a crucial role in identifying suitable patients for various treatments. This streamlined approach enabled faster diagnoses, quicker referrals, and ultimately, better patient experiences.
An excellent example of this collaboration in action was the mild® Procedure, a minimally invasive technique for treating lumbar spinal stenosis. This procedure served as a catalyst for discussions that led to deeper understanding and synergy between pain management and surgical interventions. With shared imaging interpretation and a clear algorithmic approach, the team was able to offer patients tailored solutions that ranged from minimally invasive interventions to spinal stenosis surgery, depending on the individual case.
The success of this collaborative approach was reflected not only in patient outcomes but also in practice growth. The combined efforts of pain management and surgical teams resulted in an increased patient volume, dispelling the notion that collaboration might hinder individual specialties. Instead, it enhanced the quality of care across the board.
The success story of Dr. Stevenson, Dr. Antony, and their team serves as an example for all medical professionals seeking to bridge the gap between specialties. The barriers that once stood between pain management and surgical intervention are now seen for what they truly are—perceived limitations that can be dismantled through open dialogue, shared expertise, and a genuine commitment to patient well-being. Through collaborative efforts, the medical community can continue to optimize patient care and shape a brighter future for all.
To hear more about this collaboration in action, from Drs. Antony and Stevenson themselves, please click the link below to listen to “The Pain Physician & Spine Surgeon Relationship” on ASPN’s Pain Unfiltered podcast.
Listen to the Full Podcast Here About Dr. Ajay Antony
About Dr. Ajay Antony
Dr. Ajay Antony is an interventional pain physician, working at The Orthopedic Institute after 4 years as a faculty member at the University of Florida (UF). He earned his bachelor of science at the University of Florida and earned his medical degree at St. George University School of Medicine. He went on to complete his anesthesiology residency and pain medicine fellowship training at UF. After joining the faculty, Dr. Antony served to: grow the fellowship program to national recognition, bring several new procedures to the Florida community, and continue to be a recognized leader in his specialty. Dr. Antony is a member of many professional academic societies such as the Alpha Omega Alpha Honor Medical Society, the North American Neuromodulation Society (NANS), and the International Neuromodulation Society (INS). He has lectured both nationally and internationally and teaches national training courses for fellows and practicing physicians.

About Dr. John Stevenson
Dr. John Stevenson is a board-certified neurosurgeon who specializes in spine surgery, working at The Orthopedic Institute. Dr. Stevenson became a neurosurgeon because of his love for neuroscience and the influence of his father. He received his undergraduate education at Oberlin College and his medical training at the University of Glasgow. He then went on to complete his residency training in neurosurgery at Duke University Medical Center. Dr. Stevenson is a member of numerous professional associations, some of which include The American Association of Neurological Surgeons, Fellow of the Royal College of Surgeons of England, and the Congress of Neurological Surgeons.
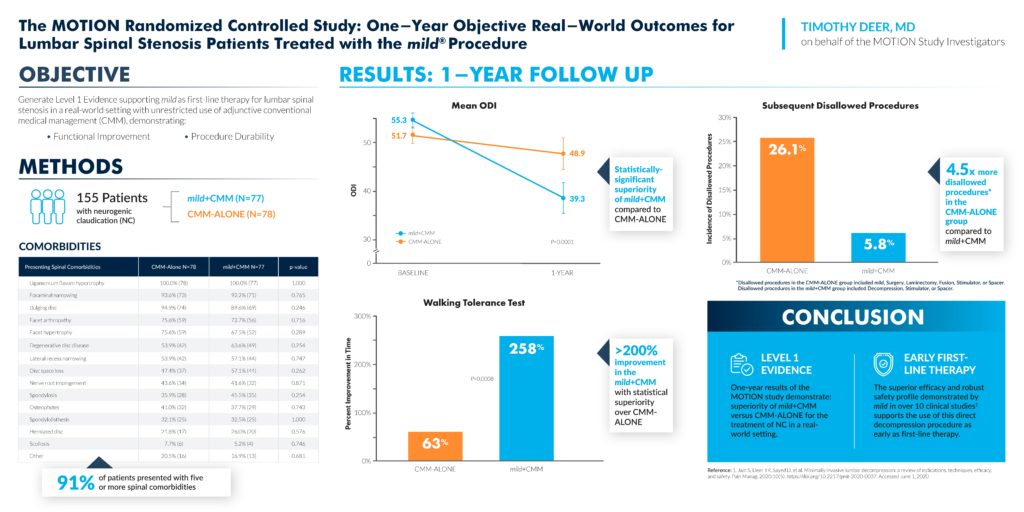
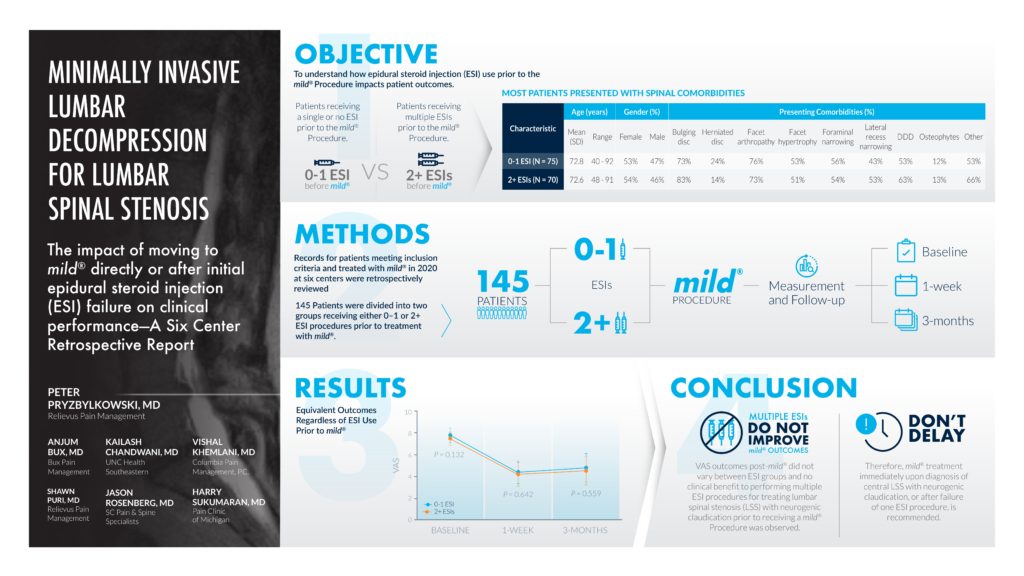
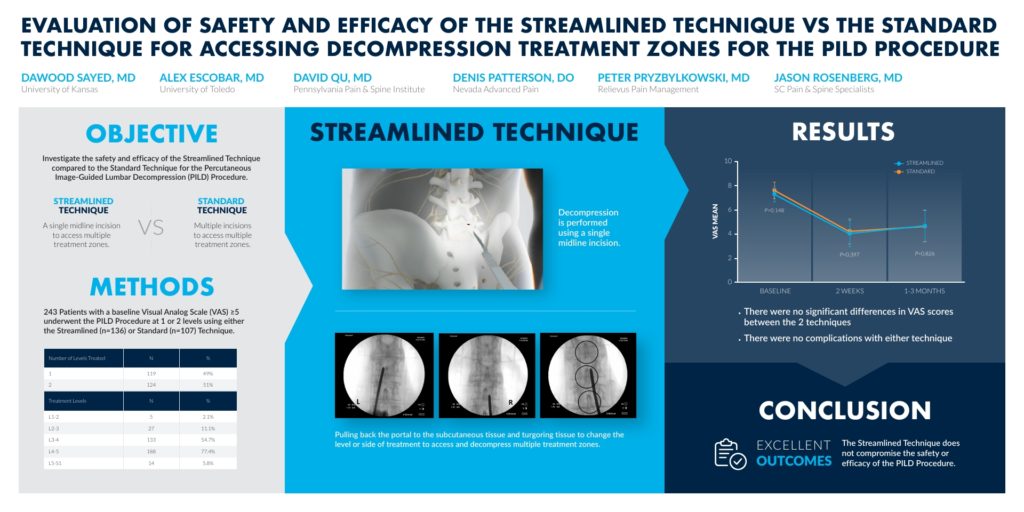
In July 2023, the American Society of Pain and Neuroscience (ASPN) held its 5th annual conference in Miami Beach, FL. The society’s goal is to facilitate the role of evidence-based pain medicine research, patient education, and advocacy, and to continue to be on the cutting edge of pain medicine interventions. As part of the conference, a number of abstracts showcased the mild® Procedure, a minimally invasive procedure that debulks thickened ligament in the spinal canal to address a major root cause of lumbar spinal stenosis (LSS). Below are the featured abstracts and their summaries.
Please view the abstracts to review their associated clinical data.
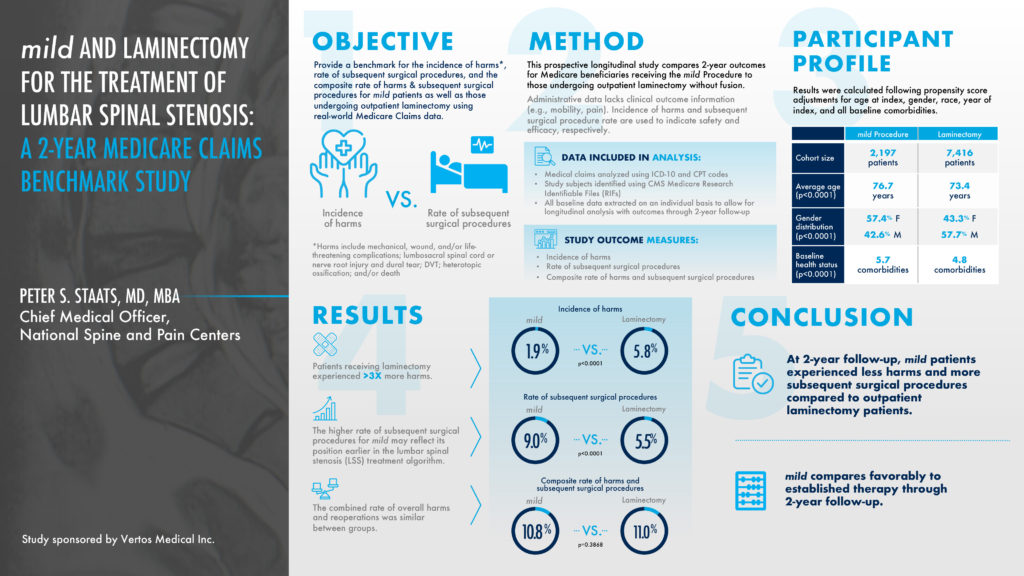
WINNER — Selected as an ASPN Top Abstract 2023
This prospective longitudinal study compared 2-year outcomes for Medicare beneficiaries receiving the mild® Procedure to those undergoing an outpatient laminectomy, a type of spinal surgery. The objective was to provide a benchmark for the incidence of harms versus the rate of subsequent spinal surgical procedures. Patients receiving a laminectomy experienced 3 times more harms at a 5.8% rate, compared to a 1.9% rate for the mild® Procedure. At a 2-year follow-up, mild® patients experienced less harms and more subsequent spinal stenosis surgical procedures compared to outpatient laminectomy patients. The higher rate of subsequent surgical procedures for mild® may reflect its position earlier in the lumbar spinal stenosis treatment algorithm.
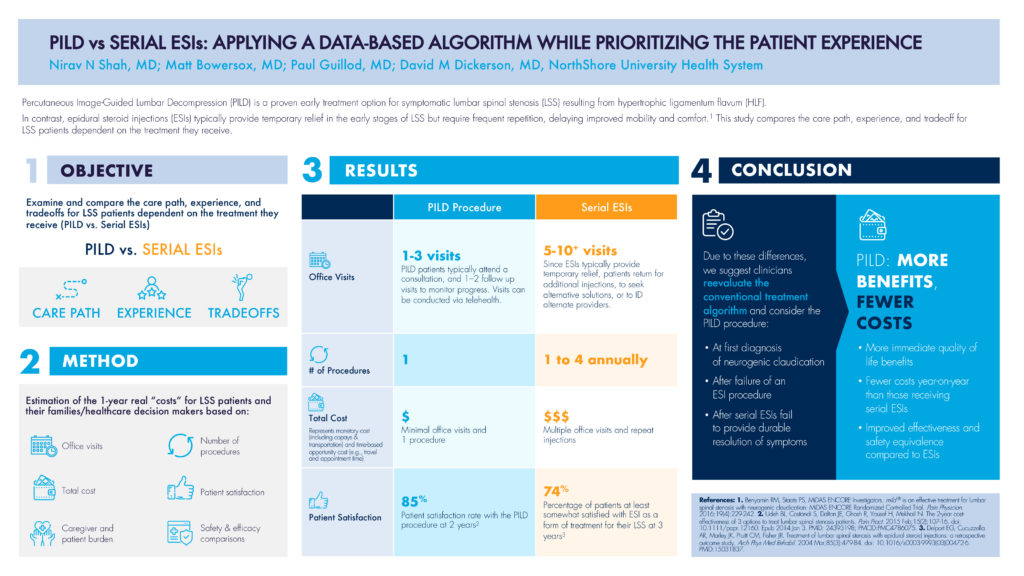
This abstract’s objective was to examine and compare the care path, experience, and tradeoff for LSS patients dependent on the treatment they receive, comparing PILD to serial ESIs (epidural steroid injections). As highlighted in the abstract, Percutaneous Image-Guided Lumbar Decompression (PILD) is a proven early treatment option for symptomatic lumbar spinal stenosis resulting from hypertrophic ligamentum flavum (HLF). In contrast, epidural steroid injections (ESIs) typically provide temporary relief in the early stages of LSS but require frequent repetition, delaying improved mobility and comfort. The methodology estimated the 1-year real “costs” for LSS patients including the number of office visits, the number of procedures, the total cost, and patient satisfaction, to name a few.
In terms of office visits, PILD patients typically attend 1—3 visits including a consultation and follow-up visit, whereas serial ESI patients often return for additional injections, increasing their total number of visits to the 5—10+ range. The total cost of multiple visits shows a three-time multiplier for serial ESI patients compared to PILD patients, where the total cost represents both monetary costs like co-pays and transportation, and the time-based opportunity cost such as travel and appointment time. Even the patient satisfaction rate for PILD patients was 11% higher compared to serial ESI patients, 85%—74%.
Due to these differences, PILD offers more patient-centric benefits and fewer costs, and would be recommended:
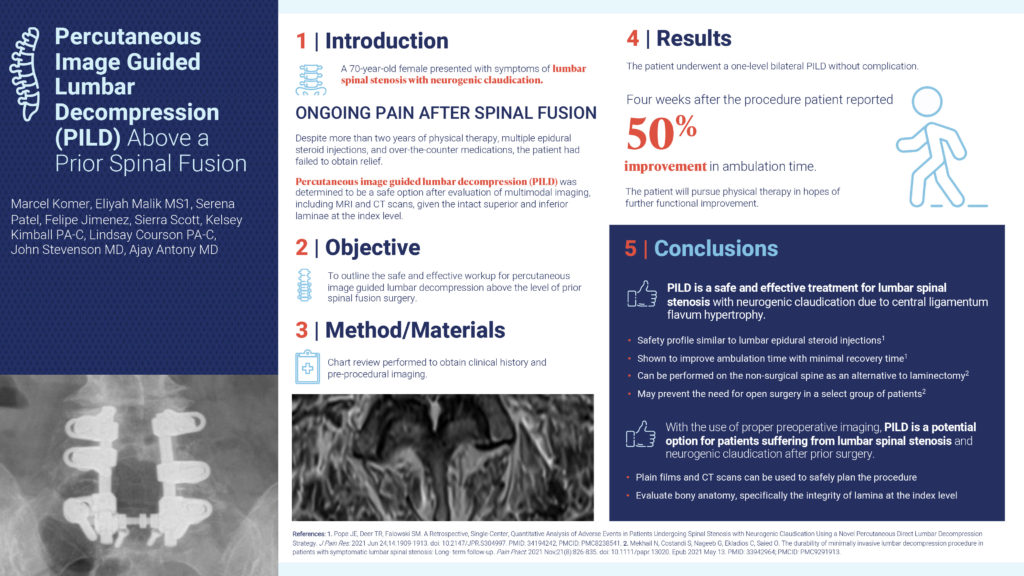
This abstract’s objective was to outline the safe and effective workup for percutaneous image guided lumbar decompression above the level of a prior spinal fusion surgery. In this case study, a 70-year-old female presented with symptoms of lumbar spinal stenosis with neurogenic claudication and felt ongoing pain after a spinal fusion. Despite more than 2 years of physical therapy, multiple epidural steroid injections, and over-the-counter medications, the patient had failed to obtain relief. After an evaluation of MRI and CT scans, the patient underwent a one-level bilateral PILD without complication. Four weeks after the procedure, the patient reported a 50% improvement in ambulation time. In conclusion, with the use of proper preoperative imaging, PILD is a potential option for patients suffering from lumbar spinal stenosis and neurogenic claudication after prior surgery.
This abstract’s objective was to create an approach by which pain practices can increase surgical referrals for PILD by collaborating with surgeon practices, and ultimately optimizing patient care. PILD is an ideal procedure to foster surgeon collaboration since it provides a treatment option for nonsurgical candidates and keeps patient in the practice. Surgical Advanced Practice Providers (APPs) are therefore an ideal PILD referral source as they are familiar with patient histories, have the exposure to nonsurgical candidates, and are eager to optimize patient care. If APPs have knowledge of PILD as a potential treatment, suggesting it as a first option for these nonsurgical patients and collaborating with Interventional Pain Management (IPM) would become routine and enhance patient care.

Authors’ Affiliation
*Novant Spine Specialists, Charlotte, NC, USA
**California University of Science and Medicine, CA, USA
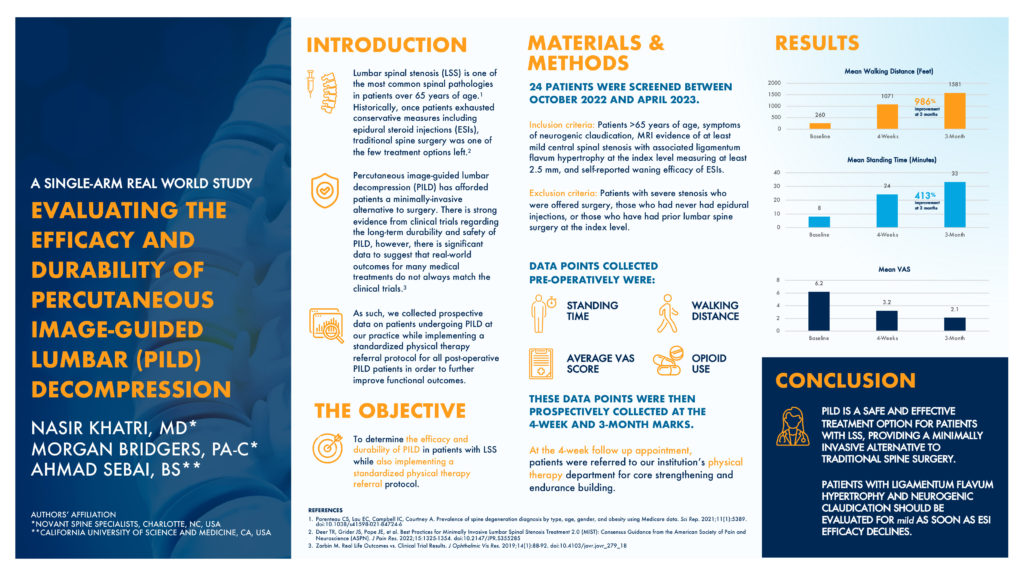
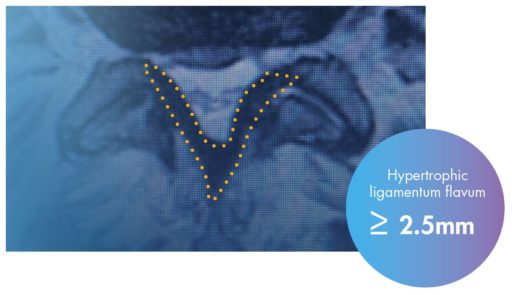
This abstract’s objective was to determine the efficacy and durability of PILD in patients with lumbar spinal stenosis while also implementing a standardized physical therapy referral protocol. These patients were older than 65 years old, with symptoms of neurogenic claudication. They had MRI evidence of at least mild central spinal stenosis with associated ligamentum flavum hypertrophy measuring at least 2.5mm, with a self-reported waning efficacy of epidural steroid injection results. Data points such as standing time and walking distance were collected at a baseline timeframe and 4 weeks post-operatively. At the 4-week follow-up appointment, patients were also referred to a physical therapy routine for core strengthening and endurance building. At the 3-month follow-up, the mean walking distance showed a 986% improvement and the mean standing time showed a 413% improvement. Abstract authors conclude that PILD is a safe and effective treatment option for patients with lumbar spinal stenosis, providing a minimally invasive alternative to traditional spine surgery.
The views and opinions expressed in this article are those of the authors/speakers and do not necessarily reflect the official policy or position of Vertos Medical.

We’re proud to highlight Ashley Comer, A.P.R.N., NP-C, on her educational Op-Ed article in the Charleston Gazette! As a member of our Advanced Practice Provider (APP) Advisory Board and as a nurse practitioner working within Interventional Pain Management (IPM), Ashley interacts daily with patients suffering from chronic low back pain (CLBP), many of whom are simply searching for relief.
Data from a recent Harris Poll survey found that nearly 3 out of every 10 US adults currently suffer from CLBP, and over a third of those surveyed rated their back pain as “severe.” Many of these individuals visited multiple doctors, and while their pain progressed, only then considered seeing an Interventional Pain Specialist.
Read Ashley’s insights below on why patients should consider IPM at the onset of pain treatment and potential treatment options outside of the often-prescribed opioids.
View Full Publication
As an Advanced Practice Provider (APP), you are an integral part in helping patients with lumbar spinal stenosis (LSS) get on the path to lasting relief.
In this webinar workshop, led by our panel of mild® experts, APPs Ashley Comer, NP, Marie Zambelli, NP, Kelsey Kimball, PA, Lauren Cote, NP, Patrick McGinn, PA, Kristen Klein, NP, discuss how patient education and proper outcomes assessment play an important role in optimizing patient outcomes after the mild® Procedure.
Access the webinar here:
Looking for more info on mild® patient identification criteria?
Check out our blog: Identifying & Educating mild® Patients – APP Guidance
Sign up to stay informed and receive the latest updates!
Sign Up NowAccording to our Advanced Practice Provider (APP) Advisory Board, imaging review, a key aspect of mild® patient candidate identification, is often not included in initial schooling. To help APPs learn the basics of image review, become more familiar with identifying anatomical landmarks, and understand how to confirm if a patient is a candidate for the mild® Procedure, we asked James Lynch—an APP with the Pain Consultants of San Diego—to walk us through his tips and techniques for magnetic resonance imaging (MRI) review. In the following article, he shares pearls for becoming confident in imaging review and provides a series of videos so you can follow his step-by-step approach to determine if patients with lumbar spinal stenosis (LSS) should make the move to mild®.
As an APP in an Interventional Pain Medicine practice that offers the mild® Procedure, reviewing MRI images to determine the presence of hypertrophic ligamentum flavum (HLF) is a critical aspect of my role. Prior to joining this practice, I had very little experience reviewing MRI images. It was not part of the core curriculum while training to become an APP, and it was not an area that I felt very confident in. I’ve become more familiar and proficient with imaging review; however, I can say that it’s much more straightforward than it may initially seem. Through hands-on experience, by sharing clinical pearls among peers, and by watching step-by-step videos like those included in this article, I became competent, comfortable, and confident performing image reviews to identify mild® patient candidates—and I know other APPs can too.
We know that up to 85% of spinal canal narrowing is caused by thickened ligament. When we see patients with symptomatic LSS, if HLF is present, we will likely advance to mild® to provide patients long-term relief using a therapy that has a safety profile equivalent to an epidural steroid injection (ESI), but with lasting results. Being able to review a basic MRI empowers me to identify patients who may benefit from the mild® Procedure and confidently present my recommendations to them. This confidence helps build trust between me and my patients, and makes them feel more comfortable and assured prior to scheduling their mild® Procedure. Having more patients move to mild® means that I’m giving my patients a chance to achieve clinically meaningful, statistically significant improvements in mobility, Oswestry Disability Index (ODI), and pain reduction on the Numeric Pain Rating Scale (NPRS). It’s also incredibly rewarding to hear patients tell me about what they’re able to do now that they can walk further and do more activities than they could before.
LSS is highly recognizable by the signs and symptoms patients commonly exhibit, including pain, numbness, or heaviness when standing or walking, and finding relief by sitting, bending forward, or sleeping curled in the fetal position. When we see these signs in our patients, we’ll order an MRI to confirm the diagnosis and determine whether the patient is a good candidate for the mild® Procedure.
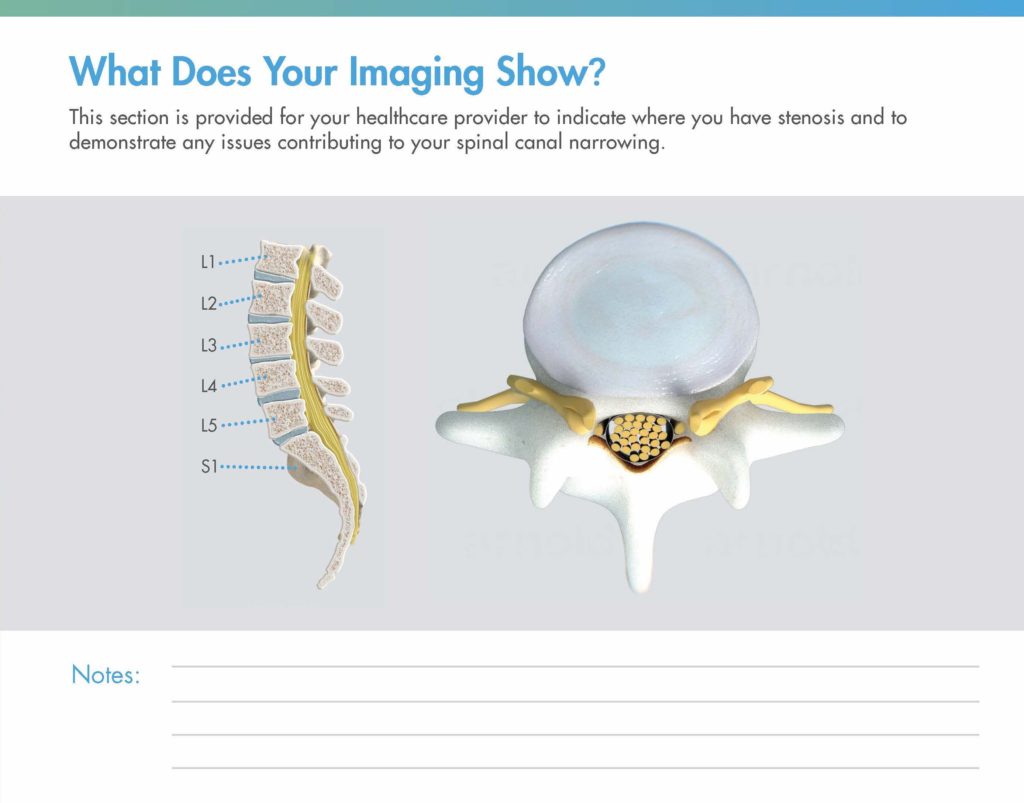
When we request an MRI, we’ll get a report and the imaging back for that patient. During my review of the report, I look line-by-line, specifically confirming whether the report notes central canal stenosis. It is also helpful to make note of other contributors to central canal stenosis (such as enlarged facets, disc bulge, etc.) in order to properly prepare a patient for potential follow-up expectations.

Tip: As you gain comfort with image review, practice reviewing the MRI first and report second to confirm their diagnoses.
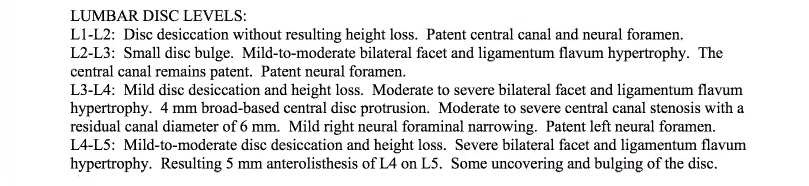
In the example shown here, I would note the following:

Reminder: You can also request that the radiology report include a measurement of the HLF, which can make it easier to review.
Because I have confirmed the presence of central canal stenosis in the report, I’ll then review the imaging to determine whether the patient is a candidate for the mild® Procedure. You can also take the reverse approach and review the imaging first, and then use the radiology report as a confirmation of your own findings.
A note on software: While the specific software demonstrated in this blog is Ambra Health, much of the imaging software used today is similar in function and review procedures. Whether you’re using Ambra Health, Sharp, or another software option, the tips and tricks demonstrated in this blog should be consistent, regardless of the software you’re using.
In pulling up the images, I typically begin setting up the images to facilitate a clear and efficient review process. Begin by adjusting the layout of the software to show 2 images at the same time.
On the left-hand side, we will show the sagittal view, or vertical cross-section of the patient. On the right-hand side, the axial view, or horizontal cross-section of the patient, will be displayed.
Press the “Link” command in the system software to correlate the images together and select the STIR images (T2 weighted images).

Tip: The reason I use the T2 image is because the cerebral spinal fluid actually brightens up, making it a lot easier to assess the spinal canal.
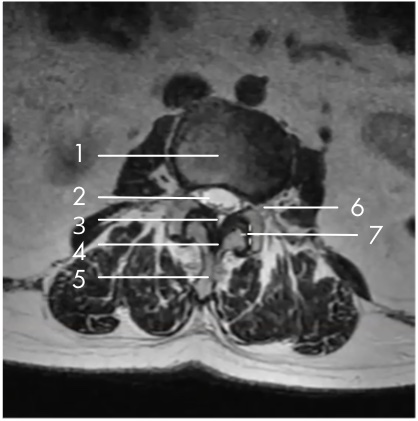

My specific area of interest in evaluating the mild® patient candidate is the small black area, which is the ligamentum flavum, highlighted in the image here.
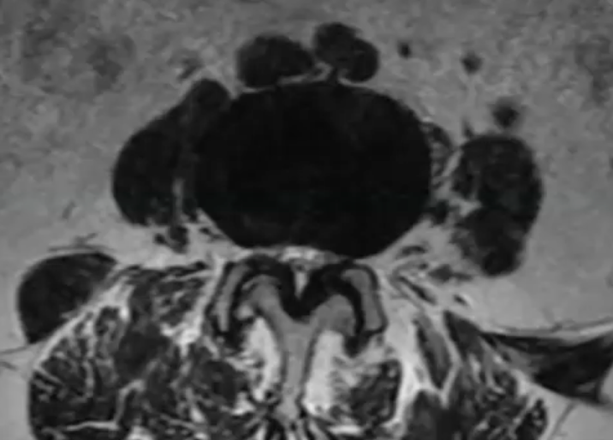
In the small white area, we can see the central canal where the nerves are housed. In this image, we can see that the canal is very small, with very little white showing. This is consistent with central canal stenosis, and in this case, we can see clearly that the hypertrophic ligamentum flavum is compressing the nerves.
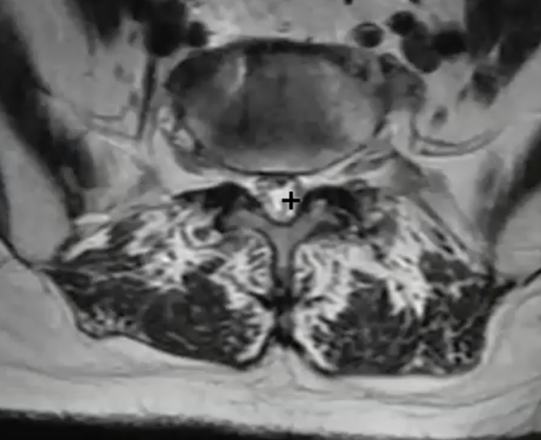
By moving our image up to L2-L3, we can see an excellent comparison of the healthy central canal. The large white area shows that at this level, the thin black ligament is not compressing the nerves.
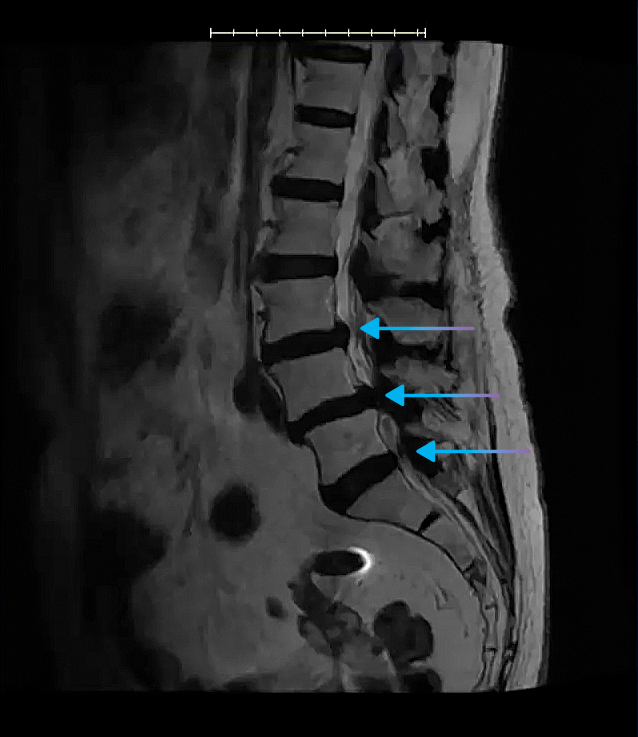
In the sagittal view, you’ll be able to see clearly where the spinal canal narrows, and this is helpful in identifying all levels where the central canal is stenosed.
We can also see here that the patient has a disc bulge, indicative of multi-factorial central canal stenosis.
It’s important to remember that comorbidities are common among LSS patients—in fact, a Level-1 clinical study of mild® patients demonstrated that just 5% of patients presented with central canal stenosis only. The presence of comorbidities, such as foraminal narrowing, lateral recess narrowing, or facet hypertrophy DO NOT RULE OUT patients as mild® Procedure candidates. Indeed, the same clinical study found that the majority of patients with comorbidities achieved an ODI improvement of ≥10 points at 2-year follow-up.
Using the length tool in the software, I can draw a line across the ligament (the dark area indicated in the image below) to obtain the ligament measurement.
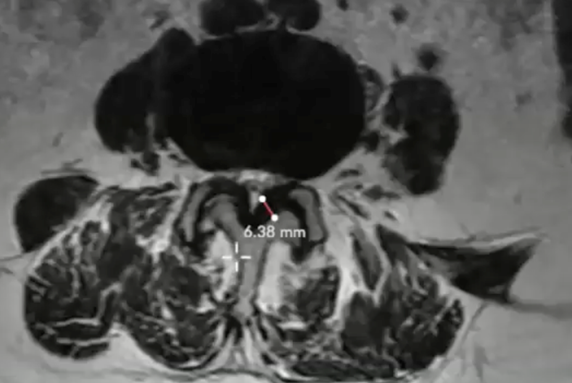
Here, the measurement clearly shows an HLF of 6.38 mm. I will then repeat this measurement process at each of the levels that are affected by central stenosis (per the report, and as seen in the sagittal view).

Tip: As a reminder, any patients with HLF ≥2.5 mm may be considered a candidate for the mild® Procedure.
Once you become familiar with imaging review, you’ll develop your own tips and tricks that make the process easier and more efficient for you. Here are a few things that I suggest that can help when you’re just getting started:
In this video, you can see an end-to-end example of the imaging review for an ideal mild® case. In under 5 minutes, you can see how I:
When a patient can’t have an MRI, we will instead send them in for a computed tomography (CT), ideally with a myelogram. A myelogram will highlight these relevant anatomical structures, so you can see the ligament and determine the patient’s candidacy. Even if a myelogram is not an option, be sure to indicate a primary diagnosis for lumbar stenosis when you order the CT, and the radiologist will then assess that patient for lumbar stenosis and HLF.
When patients are in the office, I’ll often bring my laptop into the exam room and show them their imaging on screen. Being able to see their own anatomy, and specifically the hypertrophic ligament pressing on the nerves, is incredibly helpful to demonstrate this root cause of their LSS.
Then, I can also use the imaging to clearly point out how mild® addresses a major root cause of LSS by removing excess ligament tissue and leaving no implants behind. I’ll also show them where the nerves are being compressed and educate them about how mild® restores space in the spinal canal, which reduces the compression of the nerves. Most patients understand how the mild® Procedure works much more easily when they can see the images themselves, and it also helps them realize how the mild® Procedure can provide long-term relief and restore mobility.
When I first started with imaging review, I was much less comfortable and confident than I am today. Knowing that our practice is committed to helping more patients move to mild®, I recognized that becoming comfortable with imaging review was a critical aspect of my role. Even though MRI review was not something included in my initial APP education, I realized that becoming proficient gave me an opportunity to bring additional value to our patients and practice.
The best way I found to get comfortable with imaging review was to dive in and review previous cases so I could become familiar with the anatomy and structures. Beyond hands-on experience, there are resources that offer additional support, including:
With additional practice and experience, you’ll quickly become much more comfortable with imaging review. You’ll also notice how many of your patients with LSS have HLF and are candidates for the mild® Procedure. By putting more patients on the path to lasting relief with mild®, you’ll get to see first-hand how regaining mobility can be a life-changing improvement for the patients in your care.
Advanced Practice Providers (APPs) play a vital role in helping patients understand their lumbar spinal stenosis (LSS) diagnosis and treatment recommendations. By developing strong provider-patient communication, you’re taking the first step towards achieving positive outcomes and enhancing the patient experience.
Why is patient education so important?
Based on the data above, it is clear that patients over 65 years of age–the group most likely to suffer from LSS–may need more support to understand their condition and treatment plan. With the recognition that both lumbar spinal stenosis and poor health literacy can increase your patients’ susceptibility to poor physical functioning, pain, and limitations in activities of daily living, APPs should feel especially empowered to engage patients. This includes helpful education and dialogue that supports their understanding and helps them feel more comfortable taking the next step on their path to lasting relief.
In the following article, you will find step-by-step guidance and pragmatic suggestions that you can start using today, to help you ensure that your patients leave their consultation feeling confident and excited about their opportunity to make the move to mild®.
Watch: See APP Ashley Comer’s complete talk track for presenting mild® to her LSS patients.
Use the mild® patient brochure as a tool and follow these simple steps to help your patients better understand their lumbar spinal stenosis diagnosis and the benefits of the mild® Procedure.
![]()
Instead of using complex medical terms or acronyms, simplify your explanation with common words, phrases, and analogies to help patients understand their diagnosis and treatment options.
According to the CDC, nearly 9 out of 10 adults struggle to understand and use personal health information when it’s filled with unfamiliar or complex terms. (Source)
On the first page of the mild® patient brochure, you’ll find helpful illustrations that demonstrate the anatomical changes associated with LSS and the symptoms patients typically experience. During your patient consultation, be sure to highlight:
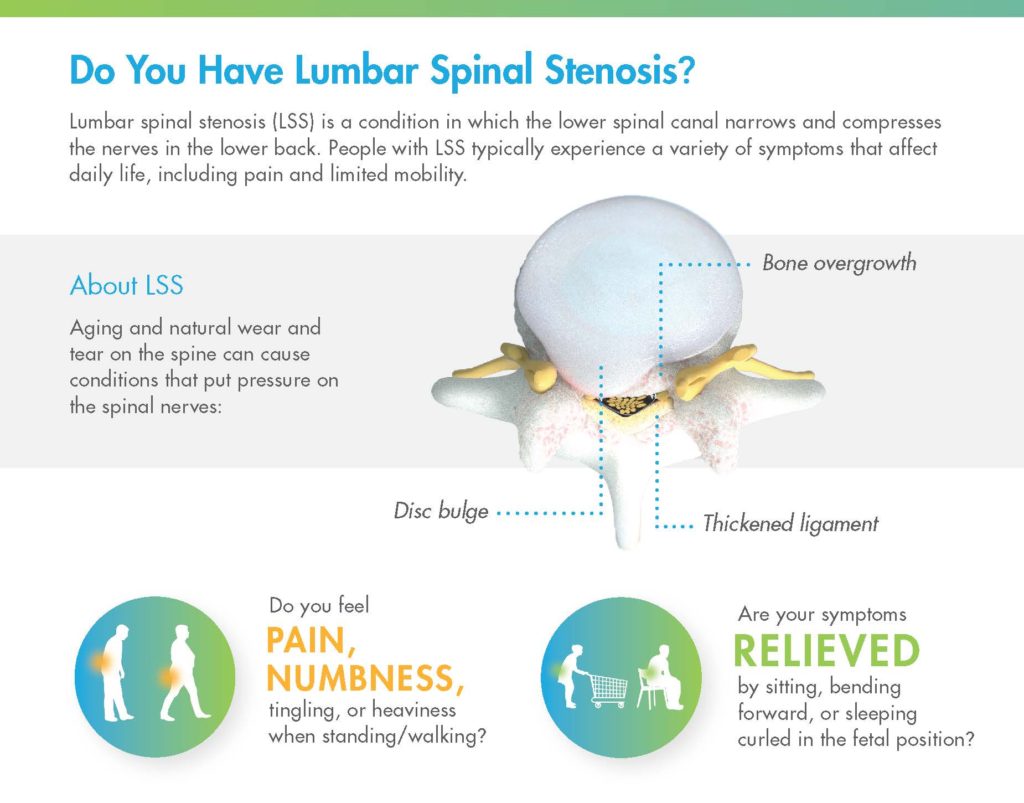
![]()
Many APPs and physicians use common, real-life analogies to help patients identify and understand their LSS symptoms. A common analogy that many patients may relate to is the “shopping cart syndrome.” Explaining that patients with lumbar spinal stenosis often feel relief when bending over a shopping cart (because it reduces pressure on the compressed nerves) can help patients recognize how this condition impacts their daily life.
Once you’ve established the common signs and symptoms of LSS, demonstrate what the MRI shows for that specific patient. Turn to the last page of the mild® patient brochure, where you can use the diagrams provided. Drawing directly on the patient brochure, indicate the following:
Watch: See how APP Ashley Comer uses the illustrations in the mild® patient brochure to demonstrate her patients’ specific areas of stenosis.
You can also accompany the spinal illustrations in the mild® patient brochure with an added tool, such as a spine model or the patient’s MRI to reinforce the anatomical positioning of the problem or validate the diagnosis, respectively.
Once patients fully understand their condition, walk them through all of the reasons why you recommend they make the move to mild®. If you turn back to the beginning of the brochure (or access the same information in the mild® patient flip chart) and review the remaining pages, you can quickly cover the advantages of mild® relative to other treatment options, and prepare your patients for what to expect during and after their mild® Procedure.
Because epidural steroid injections (ESIs) were historically the standard of care for lumbar spinal stenosis patients, your patient may be expecting you to recommend another injection. You can explain that the data shows that there is no benefit to giving more than one ESI before mild®, and that giving more than one ESI delays the patient from receiving the longer-lasting, more effective mild® Procedure.

![]()
Every year, thousands of lumbar spinal stenosis patients are able to stand longer and walk farther with less pain thanks to the mild® Procedure, but those results aren’t achieved overnight. Improvements in patient functionality are typically achieved over time, with patients gradually increasing standing time and walking distance. If you set expectations in advance, patients may be more excited and satisfied to see their own functional improvements over time.
LSS patients rely on APPs as critical members of their care team. Across the patient journey from diagnosing your patients’ LSS to finding relief with the mild® Procedure, APPs are key in supporting patients, helping them understand their condition, and feeling confident about their decision to make the move to mild®.
At Vertos, we recognize and support the role of APPs and are committed to providing education and resources that help you put more LSS patients on the path to lasting relief.
Don’t miss out on the latest and greatest tips and tools from Vertos.
mild® is often referred to as a “simple little procedure” that can make a major impact on the quality of life and mobility for lumbar spinal stenosis (LSS) patients. Minimally invasive lumbar decompression (mild®) removes the problem and leaves nothing behind—no implants, no stitches—allowing patients to stand longer and walk farther with less pain. A short, outpatient procedure, it is performed through a single 5.1mm incision in the patient’s lower back, addressing a major root cause of lumbar spinal stenosis by removing excess ligament tissue. Patients typically resume normal activity within 24 hours with no restrictions.
So, how do practices describe this “simple little procedure” to their patients? We like to say the mild® Procedure is similar to “removing a kink in a drinking straw,” reducing the compression on the nerves in the lower back to restore mobility and relieve pain.
We asked a group of mild® physicians how they describe the mild® Procedure and its big, life-changing potential to their patients and referring physicians. We heard a lot of fun analogies—here are a few of our favorites.

I describe mild® to my patients as a “quality-of-life procedure.”
I walk them through my algorithm and I say, “Listen: I can put a temporary Band-Aid [solution] on this for you with an epidural steroid injection (ESI), or I have a tool in my toolkit that could hopefully fix this for you where it’s not just a Band-Aid. It really improves your quality of life.”
Once you frame it this way for patients—as an epidural being a Band-Aid, with mild® being more of a definitive procedure—you have a captive audience that typically wants to go ahead and get a percutaneous decompression.
Our patients are generally familiar with cardiology procedures. So, I tell them lumbar spinal stenosis treatment options are similar to the options available for patients with coronary artery stenosis. You can either treat them with meds to improve blood flow or put in a stent to open it up more permanently. The mild® Procedure restores space around the spinal cord, just like a stent restores space in your blood vessels.
I tell patients: “Your spinal canal is kind of like your sink when it gets clogged. If your sink is really clogged, you can pour Drano down it all you want. But that’s a temporary fix, and it doesn’t work long-term. At some point, you’ve got to get in and unclog the drain.”
I describe how mild® works like fixing a room that is overcrowded with furniture. I tell them:
“Imagine a room full of tables and chairs, and you just can’t move around. What I am going to do today is just take a couple of chairs out to make some more space, so your anatomical structures can move around easily.”
“When I describe what stenosis/LSS does to a patient’s spinal canal, I compare it to having too many people in an elevator. What we do with mild® is open the door and let a few people out so that the folks remaining have more room to move freely for the ride.”
How do you describe mild® to your patients? If you have an effective analogy you use to talk about the benefits of mild® or its approach, we’d love to hear about it. Email us today. If you need additional patient resources, please contact your Vertos representative.
As a mild® provider, it’s important to brand yourself as a mild® practice to attract new patients and educate people in your community who are searching for relief from lower back pain and mobility issues. By presenting the mild® Procedure as part of your treatment offerings, you can highlight that your practice provides advanced lumbar spinal stenosis (LSS) treatment options for potential patients searching for alternative solutions to epidural steroid injections (ESIs), pain medication, or back surgery.
The following patient education, healthcare professional, and digital (web/social) resources will help ensure your practice is well-equipped in identifying and educating the community and your referral networks about LSS, and how mild® can play an effective role in a patient’s care path.
Outfit your practice so patients know you offer the mild® Procedure.
Add information about mild® to your website to help educate patients about the procedure.
Additional content and tools designed specifically for APPs to help identify and educate patients.
Build connections with referring physicians to help attract more patients to your practice.
Word-of-mouth can be one of the most powerful tools to grow your mild® practice. Encourage patients to help advocate on your behalf.
We’re here to help! Team Vertos is committed to ensuring your practice has a strong foundation of tools to educate your community about the mild® Procedure and how its benefits are transforming the lives of patients. Please reach out if you need further assistance in optimizing these resources.
To order patient education marketing materials (brochures, posters, etc.) or to schedule a staff training, please contact your local Vertos representative.
For additional marketing-related questions, please email us at mild@vertosmed.com.
Interventional Pain Management is a fast-growing specialty. As new lumbar spinal stenosis (LSS) procedures become available, practices are evolving the way they collaborate and work together to optimize patient care. The mild® Procedure’s patient selection process is quite simple, but requires imaging review, which is often not a part of Advanced Practice Providers’ (APP) traditional education.
Although image review can be intimidating, APPs report that the learning curve is relatively short and there are resources available to help you get started. Below are some tips from mild® APPs on how they quickly established comfort with imaging review in their practice, allowing them to “look for the ligament,” identify hypertrophic ligamentum flavum (HLF), and educate mild® patients independently.

In a prior CME webinar hosted by the American Society of Pain & Neuroscience (ASPN), moderators Timothy Deer, MD; Dawood Sayed, MD and faculty members Navdeep Jassal, MD; Eugene Paik, MD; Ashley Comer, NP-C; Christine Christensen, APRN; and Zohra Hussaini, MSN, FNP-BC, MBA, APRN discussed how physicians and APPs can match more patients with the right treatments sooner by working together.
Visit ASPN’s websiteLooking for more info on mild® patient identification criteria? Check out our blog: Identifying & Educating mild® Patients – APP Guidance. Interested in APP-focused education and events? Sign up to stay informed and receive the latest updates!
Sign Up NowWe know that mild® is a great option for the lumbar spinal stenosis (LSS) patients in your practice—but it’s also a great way to differentiate your offering and attract more referrals from the community.
As mild® has gained more and more momentum—demonstrating a safety profile equivalent to epidural steroid injections, positive patient outcomes, and 5-year durability of results—our practice has made mild® a cornerstone of our LSS treatment algorithm. It’s certainly rewarding to see patients regain mobility and get back on their feet. Importantly, when these cases become success stories, mild® patients, their family members, referring physicians, or physical therapists become powerful advocates in the community, driving referrals and offering compelling testimonials that build credibility, motivate new patients, and improve your community’s access to this meaningful treatment.
It’s important to recognize that today, many people in our communities still think about pain management in terms of medications and epidurals. As interventionalists, we have an opportunity to educate them on the wide range of services we provide and how we can not only help manage symptoms, but also restore function, improve overall health, and enhance overall quality of life. If the mild® Procedure has yet to become part of your management of lumbar spinal stenosis (LSS), my colleagues share in a recent blog post how to integrate the procedure into an LSS treatment algorithm. Here are a few steps you should consider taking to reach and attract more patients:
As clinicians, we are often tasked with making complex concepts accessible to our patients and other clinicians, many of whom only know LSS as “chronic low back pain” or who believe options are limited to serial epidural steroid injections or surgery.
To introduce mild®, we utilize the patient education tools to emphasize several key points:
If they ask why our practice moves to mild® early in the treatment algorithm, we can reference this recent clinical study, published in Pain Management, which found that:
To help patients and caregivers access and engage with this information, I like to share a plain language summary document. It helps patients better understand how mild® can reduce the treatment burdens associated with frequent injections, provide lasting therapeutic results, and help our practice meet our primary goal of restoring function and achieving sustained improvement in quality of life.

We also use the summary to educate and build relationships with referring clinicians, many of whom are unfamiliar with minimally invasive lumbar decompression, the procedure, and its impact on care protocols. The summary is written using simple language but is very detail-rich, making it a valuable resource for health stakeholders involved in collaborative care. When we send this to practices in our network, we like to strengthen the referring relationship by:
In addition to sharing the plain language summary, it can be helpful to leverage educational videos on your website to further inform patients about the benefits of mild® for lumbar spinal stenosis.
To help patients find the information they’re looking for, create a video summary that describes the information the patient is about to see. The shorter and more concise the description, the better. You can include specific details on the benefits of mild® leading with the key points patients care most about:
Success stories from patients who have benefited from your spinal stenosis treatment offer a powerful and influential tool for creating patient awareness and should form a cornerstone of your outreach efforts. When a patient finally finds relief, they usually want to help other people who are suffering get back on their feet.
Document your lumbar spinal stenosis patients’ treatment journeys and capture testimonials so you can share them on your website and social media platforms. Teach them how to recognize the signs of LSS in their friends and family members and encourage them to share their story.
Additionally, when working with referring care providers, implement strong post-procedure communication strategies to cultivate active, engaged partnerships. Following a mild® Procedure, we inform referring providers of their patients’ results, and help them understand what the patient can expect over time.
When APPs understand that patient functionality continues to improve as time progresses, they can help manage patient expectations. APPs working within our referring clinicians’ offices also appreciate frequent status updates. This often translates into additional patient referrals and better care partnerships.
At the end of the day, our primary goal is to offer meaningful outcomes that restore function and reduce pain for patients in our community. To capture attention and positively impact more lives, it is fundamentally important that we make our communities aware of the full range of services we offer for lumbar spinal stenosis patients.
Taking this approach takes a little work but yields considerable reward. Successfully treating with mild®, using those successes to build lasting community relationships, and helping patients finally get on the path to relief, has brought our practice immense satisfaction, as well as steady increases in patients coming in to see what options we may have to treat their pain and increase their activity.
If your lumbar spinal stenosis (LSS) treatment algorithm relies on serial epidural steroid injections (ESIs) to relieve chronic lower back and leg pain associated with neurogenic claudication, data supports a different approach—performing the mild® Procedure immediately upon diagnosis of LSS or moving to mild® after the first ESI fails may help your patients avoid “ESI Exhaustion.”
We already know that epidurals are not capable of “curing” neurogenic claudication, a major root cause of lumbar spinal stenosis which is present in 94% of patients. The steroids in the injection are believed to reduce inflammation to relieve pain; however, injections are only treating the symptoms of LSS. For long lasting relief, debulking the ligament is required. Injections results typically last less than six months. To provide ongoing relief, patients often require 2-3 injections on average per year.

Due to the temporary nature of epidural steroid injection relief, and the requirement for repeat injections, many practices encounter patients with what is increasingly becoming known as “ESI Exhaustion.” ESI Exhaustion can be spotted in patients at any stage of LSS treatment or stenosis severity. Once you start recognizing the signs of ESI Exhaustion in your lumbar spinal stenosis patients, you’ll see why so many leading clinicians are moving to mild® earlier in their treatment algorithm.
When patients experience short-term relief for a condition as challenging as LSS, it can be easy for them to become frustrated and lose hope. Patients can become tired from needing to return for repeat injections. Other patients may start to feel hopeless if the injection is not effective or if it is only effective for a very short time. It’s important to remember that LSS patients often experience debilitating pain and loss of mobility that can have a devastating impact on their quality of life.
To help your patients remain optimistic and aligned to your treatment plan, educate your new and existing LSS patients about your treatment options early. Make sure they know that there is a procedure that offers the safety equivalence of an ESI, but with lasting results. If you are starting their treatment plan with a single epidural, inform them about the mild® Procedure during that first visit, so they know that if the ESI is not effective, there are other options that can help restore mobility by addressing a major root cause of LSS.

One of the more common questions patients have about a steroid injection is “how long will the results last?” Unfortunately, with ESIs, efficacy can vary by patient, and it can be difficult to predict the degree of relief or durability of effect for each. While studies have shown pain relief for up to six months in some lumbar spinal stenosis patients receiving steroid injections, other studies have demonstrated limited effectiveness.

Even more vexing for some patients is that the durability of effect of an initial ESI may not be experienced with subsequent injections. To achieve effectiveness over two to three years, five or more injections per year may be required.
Rather than offering patients a series of injection after injection with short-term results, move to mild® after the first ESI fails. The mild® Procedure offers a clinically proven safety profile equivalent to ESIs, but with lasting results. A 5-year study completed by the Cleveland Clinic showed that mild® helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief.
If patients are dissatisfied with their results and feel they’ve run out of options in your practice, they may start to search for another solution. By offering mild® as an early intervention, you can avoid losing patients and actually increase productivity in your practice. Upon diagnosis of LSS, inform patients that you offer mild®, a minimally invasive treatment option that offers durable relief.
If you have already treated a patient with an ESI and it failed, or the patient received an injection in another practice, there is no reason to continue to offer another injection. Most patients I’ve seen are excited to learn that there is another option. Moving to mild® gives them new hope in finding lasting relief.
While “ESI Exhaustion” is highly common among LSS patients, it is also completely avoidable. Recognizing that serial injections are often the standard of care when conservative care methods like exercise and physical therapy have failed to provide relief, we published a study in Pain Management that evaluated whether LSS patients benefit from multiple ESIs prior to mild®.
The article, ‘Minimally invasive direct decompression for lumbar spinal stenosis: impact of multiple prior epidural steroid injections’ compares outcomes between 145 patients receiving either 0/1 injections or 2+ injections at 6 centers in the United States. In reviewing results between the two groups, we concluded that there is no benefit to performing multiple epidural steroid injections before the mild® Procedure and that doing so delays the patient from receiving a longer-lasting, more effective mild® treatment.
Based on this study and other favorable data, we recommend performing the mild® Procedure for lumbar spinal stenosis patients immediately upon diagnosis of neurogenic claudication with hypertrophic ligamentum flavum, or after the first ESI fails.
Does your practice offer the mild® Procedure? Do you manage patient identification and education? Follow these 3 steps to optimize your practice routine:
Shopping Cart Syndrome – lumbar spinal stenosis (LSS) with neurogenic claudication (NC). These patients will often be the first ones to find chairs in your waiting room or use the walking aids, such as a shopping cart, to establish a flexed position. The flexed posture is a common sign of NC because it opens up the spinal canal to alleviate the pressure on the central canal to avoid pain that comes with being straight, upright, or mobile.
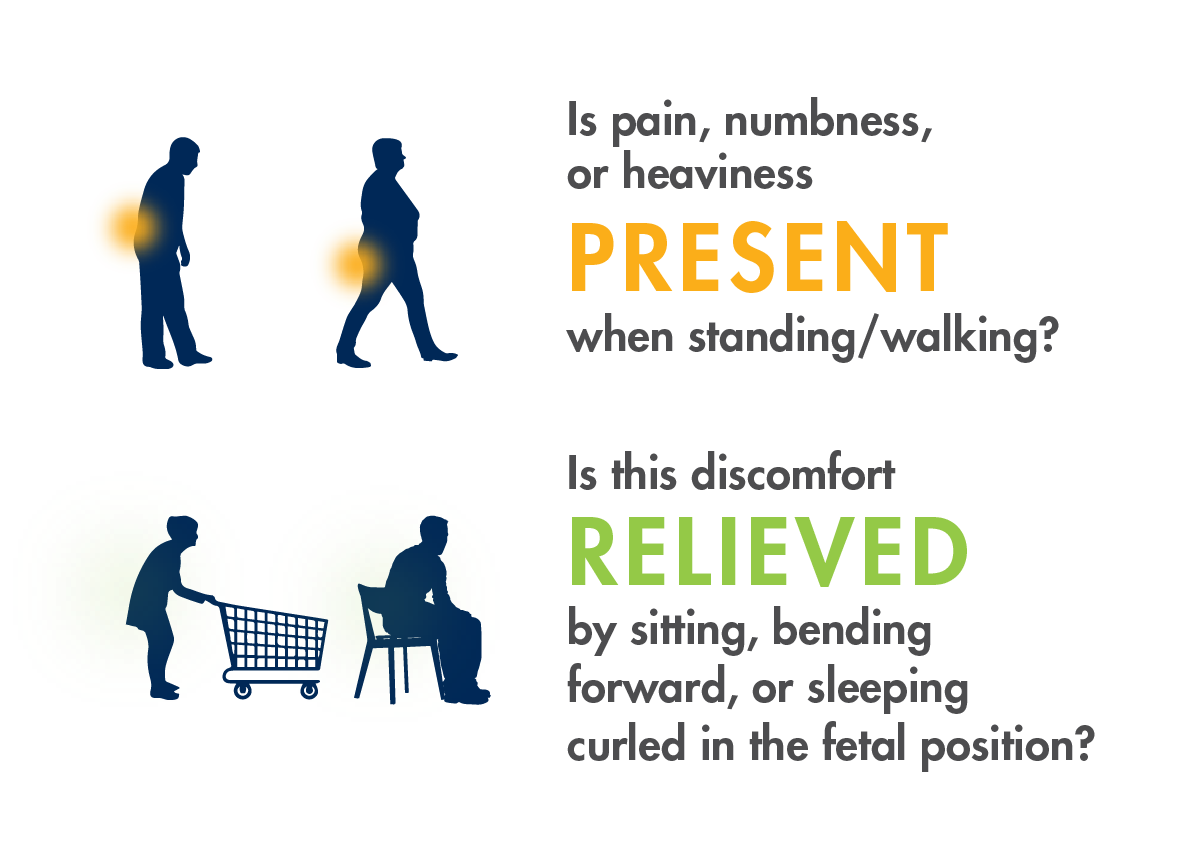
Ask patients the following questions to better understand how LSS with neurogenic claudication is limiting their mobility and when they experience symptom onset. Patients commonly report pain, so it is essential to talk about their functional limitations (eg, desire to walk the dog, get the mail, play with their grandchildren, etc.).
Consider incorporating these questions into your EMR or intake process so patients are routinely screened for neurogenic claudication.
Ask patients the following questions to better understand how LSS with neurogenic claudication is limiting their mobility and when they experience symptom onset. Patients commonly report pain, so it is essential to talk about their functional limitations (eg, desire to walk the dog, get the mail, play with their grandchildren, etc.).
Consider incorporating these questions into your EMR or intake process so patients are routinely screened for neurogenic claudication.
Hypertrophic ligamentum flavum (HLF) contributes up to 85% of spinal canal narrowing
mild® is covered by Medicare (all ages, all plan types, including Medicare Advantage), the VA, U.S. Military, and IHS. Commercial coverage varies.
![]()
mild® helps patients stand longer and walk farther with less pain.


If you would like a mild® Quick Reference Card for your office or to learn more about APP-specific educational opportunities, please contact us and let us know what you need.
What was the biggest news at the ASPN 2021 Conference? New mild® data! Five poster presentations highlight the reasons more practices are moving to mild® as a first-line therapy for lumbar spinal stenosis (LSS).
View Dr. Pryzbylkowski’s poster presentation here.
View Dr. Sayed’s poster presentation here.
View Dr. Jassal and Ms. Christensen’s poster presentation here.
Benyamin RM, Staats PS, MiDAS ENCORE Investigators. mild® is an effective treatment for lumbar spinal stenosis with neurogenic claudication: MiDAS ENCORE Randomized Controlled Trial. Pain Physician. 2016;19(4):229-242.
Mekhail N, Costandi S, Abraham B, Samuel SW. Functional and patient-reported outcomes in symptomatic lumbar spinal stenosis following percutaneous decompression. Pain Pract. 2012;12(6):417-425. doi:10.1111/j.1533-2500.2012.00565.x.
2012 data from Health Market Sciences report for Vertos Medical 2013.
Data on file with Vertos Medical.
Staats PS, Chafin TB, Golvac S, et al. Long-term safety and efficacy of minimally invasive lumbar decompression procedure for the treatment of lumbar spinal stenosis with neurogenic claudication: 2-year results of MiDAS ENCORE. Reg Anesth Pain Med. 2018;43:789-794. doi:10.1097/AAP.0000000000000868.
Based on mild® Procedure data collected in all clinical studies. Major complications are defined as dural tear and blood loss requiring transfusion.
MiDAS ENCORE responder data. On file with Vertos Medical.
Jain S, Deer TR, Sayed D, et al. Minimally invasive lumbar decompression: a review of indications, techniques, efficacy and safety. Pain Manag. 2020;10(5). https://doi.org/10.2217/pmt-2020-0037. Accessed June 1, 2020.
Deer TR, Grider JS, Pope JE, et al. The MIST Guidelines: the Lumbar Spinal Stenosis Consensus Group guidelines for minimally invasive spine treatment. Pain Pract. 2019;19(3)250-274. doi:10.1111/papr.12744.
Hansson T, Suzuki N, Hebelka H, Gaulitz A. The narrowing of the lumbar spinal canal during loaded MRI: the effects of the disc and ligamentum flavum. Eur Spine J. 2009;18(5):679-686. doi:10.1007/s00586-009-0919-7.
Treatment options shown are commonly offered once conservative therapies (e.g., physical therapy, pain medications, chiropractic) are not providing adequate relief. This is not intended to be a complete list of all treatments available. Doctors typically recommend treatments based on their safety profile, typically prioritizing low risk/less aggressive procedures before higher risk/more aggressive procedures, but will determine which treatments are appropriate for their patients.
Although the complication rate for the mild® Procedure is low, as with most surgical procedures, serious adverse events, some of which can be fatal, can occur, including heart attack, cardiac arrest (heart stops beating), stroke, and embolism (blood or fat that migrates to the lungs or heart). Other risks include infection and bleeding, spinal cord and nerve injury that can, in rare instances, cause paralysis. This procedure is not for everyone. Physicians should discuss potential risks with patients. For complete information regarding indications for use, warnings, precautions, and methods of use, please reference the devices’ Instructions for Use.
Patient stories on this website reflect the results experienced by individuals who have undergone the mild® Procedure. Patients are not compensated for their testimonial. The mild® Procedure is intended to treat lumbar spinal stenosis (LSS) caused by ligamentum flavum hypertrophy. Although patients may experience relief from the procedure, individual results may vary. Individuals may have symptoms persist or evolve or other conditions that require ongoing medication or additional treatments. Please consult with your doctor to determine if this procedure is right for you.
Reimbursement, especially coding, is dynamic and changes every year. Laws and regulations involving reimbursement are also complex and change frequently. Providers are responsible for determining medical necessity and reporting the codes that accurately describe the work that is done and the products and procedures that are furnished to patients. For this reason, Vertos Medical strongly recommends that you consult with your payers, your specialty society, or the AMA CPT regarding coding, coverage and payment.
Vertos Medical cannot guarantee coding, coverage, or payment for products or procedures. View our Billing Guide.
Vertos is an equal employment opportunity workplace committed to pursuing and hiring a diverse workforce. We strive to grow our team with highly skilled people who share our culture and values. All qualified applicants will receive consideration for employment without regard to sex, age, color, race, religion, marital status, national origin, ancestry, sexual orientation, gender identity, physical & mental disability, medical condition, genetic information, veteran status, or any other basis protected by federal, state or local law.
Hall S, Bartleson JD, Onofrio BM, Baker HL Jr, Okazaki H, O’Duffy JD. Lumbar spinal stenosis. Clinical features, diagnostic procedures, and results of surgical treatment in 68 patients. Ann Intern Med. 1985;103(2):271-275. doi:10.7326/0003-4819-103-2-271.
Kalichman L, Cole R, Kim DH, et al. Spinal stenosis prevalence & association with symptoms: The Framingham Study. Spine J. 2009;9(7):545-550. doi:10.1016/j.spinee.2009.03.005.
Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998;14(2):148-151. doi:10.1097/00002508-199806000-00010.
Mekhail N, Costandi S, Nageeb G, Ekladios C, Saied O. The durability of minimally invasive lumbar decompression procedure in patients with symptomatic lumbar spinal stenosis: Long-term follow-up [published online ahead of print, 2021 May 4]. Pain Pract. 2021;10.1111/papr.13020. doi:10.1111/papr.13020
Friedly JL, Comstock BA, Turner JA, et al. Long-Term Effects of Repeated Injections of Local Anesthetic With or Without Corticosteroid for Lumbar Spinal Stenosis: A Randomized Trial. Arch Phys Med Rehabil. 2017;98(8):1499-1507.e2. doi:10.1016/j.apmr.2017.02.029
Pope J, Deer TR, Falowski SM. A retrospective, single-center, quantitative analysis of adverse events in patients undergoing spinal stenosis with neurogenic claudication using a novel percutaneous direct lumbar decompression strategy. J Pain Res. 2021;14:1909-1913. doi: 10.2147/JPR.S304997
Pryzbylkowski P, Bux A, Chandwani K, et al. Minimally invasive direct decompression for lumbar spinal stenosis: impact of multiple prior epidural steroid injections [published online ahead of print, 2021 Aug 4]. Pain Manag. 2021;10.2217/pmt-2021-0056. doi:10.2217/pmt-2021-0056
Abstract presented at: American Society of Pain and Neuroscience Annual Conference; July 22-25, 2021; Miami Beach, FL.
Mobility Matters: Low Back Pain in America, Harris Poll Survey, 2022. View data and full summary here.
Deer TR, Grider JS, Pope JE, et al. Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST): Consensus Guidance from the American Society of Pain and Neuroscience (ASPN). J Pain Res. 2022;15:1325-1354. Published 2022 May 5. doi:10.2147/JPR.S355285.
Connect with us: Stay up-to-date with the latest information on the mild® Procedure and tag us in your posts!
Social Media Templates
Incorporate these ready-to-use social media templates into your feed. Include hashtags: #mildprocedure #vertosmedical #lookfortheligament #MOVE2mild #lumbarspinalstenosis #lss.
Now Offering mild®
We are excited to announce that we offer the minimally invasive mild® Procedure for patients with lumbar spinal stenosis (LSS). This short, outpatient treatment removes a major root cause of lumbar spinal stenosis through an incision smaller than the size of a baby aspirin and has shown to significantly improve LSS pain and mobility.
Get in touch with [PRACTICE] to see if you may be a candidate for the mild® Procedure at [PHONE #] or [WEBSITE].
Symptoms of LSS
Pain, numbness, heaviness, and tingling in the lower back, legs, or buttocks when standing or walking are common symptoms of lumbar spinal stenosis (LSS) that can make doing everyday tasks unbearable. The minimally invasive mild® Procedure addresses a major root cause of stenosis, by restoring space in the spinal canal to help improve back and leg pain.
Find out if you may benefit from the mild® Procedure by contacting [PRACTICE] at [PHONE #] or [WEBSITE] today.
Patient Education Video
A common condition typically found in those over age 50, lumbar spinal stenosis (LSS) contributes to pain and mobility issues and may impact the ability to perform simple tasks. Watch this short patient education video to learn how the minimally invasive mild® Procedure may help those with LSS achieve lasting relief.
Find out if you may benefit from the mild® Procedure by contacting [PRACTICE] at [PHONE #] or [WEBSITE] today.
Click the “Share” button on YouTube to embed the video in your social post.