In the evolving landscape of medical care, collaboration between different specialties is proving to be a game-changer for patients dealing with complex conditions. One such collaborative effort that stands out is the partnership between interventional pain physicians and spine surgeons in managing lumbar spinal stenosis (LSS). This contemporary approach aims to provide patients with a continuum of care that merges the expertise of both fields, resulting in better outcomes and improved patient experiences.
Historically, the divide between pain management and surgical intervention was palpable. However, this narrative is rapidly changing, as exemplified by the journey of Dr. Stevenson, a veteran neurosurgeon, and Dr. Antony, an interventional pain physician. Their collaboration, cautious at first, quickly evolved into a transformative model of patient care.
The key to this success lies in breaking down perceived barriers. Both specialists found that open communication, transparency, and a shared goal of patient well-being were the bridges that brought them together. Instead of focusing on the contrast between their specialties, they recognized the value of mutual learning. This synergy allowed for comprehensive discussions surrounding spinal stenosis treatment options. Topics of open discussion included MRI interpretations, indications for different procedures, and when surgery should be considered as an early option. It was a shift from a mindset of “last resort” to “best-suited solution.”
One of the most remarkable aspects of this collaboration was the way it empowered advanced practice providers (APPs), such as physician assistants (PAs), to become integral members of the patient care team. Armed with the ability to read imaging, understand evidence-based outcomes, and confidently make clinical decisions, APPs played a crucial role in identifying suitable patients for various treatments. This streamlined approach enabled faster diagnoses, quicker referrals, and ultimately, better patient experiences.
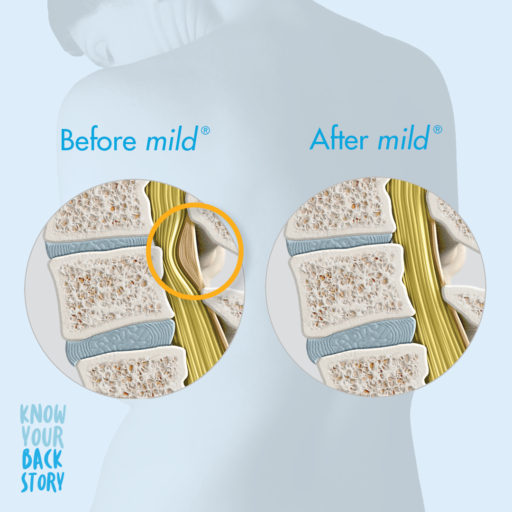
An excellent example of this collaboration in action was the mild® Procedure, a minimally invasive technique for treating lumbar spinal stenosis. This procedure served as a catalyst for discussions that led to deeper understanding and synergy between pain management and surgical interventions. With shared imaging interpretation and a clear algorithmic approach, the team was able to offer patients tailored solutions that ranged from minimally invasive interventions to spinal stenosis surgery, depending on the individual case.
The success of this collaborative approach was reflected not only in patient outcomes but also in practice growth. The combined efforts of pain management and surgical teams resulted in an increased patient volume, dispelling the notion that collaboration might hinder individual specialties. Instead, it enhanced the quality of care across the board.
The success story of Dr. Stevenson, Dr. Antony, and their team serves as an example for all medical professionals seeking to bridge the gap between specialties. The barriers that once stood between pain management and surgical intervention are now seen for what they truly are—perceived limitations that can be dismantled through open dialogue, shared expertise, and a genuine commitment to patient well-being. Through collaborative efforts, the medical community can continue to optimize patient care and shape a brighter future for all.
To hear more about this collaboration in action, from Drs. Antony and Stevenson themselves, please click the link below to listen to “The Pain Physician & Spine Surgeon Relationship” on ASPN’s Pain Unfiltered podcast.
Listen to the Full Podcast Here About Dr. Ajay Antony
About Dr. Ajay Antony
Dr. Ajay Antony is an interventional pain physician, working at The Orthopedic Institute after 4 years as a faculty member at the University of Florida (UF). He earned his bachelor of science at the University of Florida and earned his medical degree at St. George University School of Medicine. He went on to complete his anesthesiology residency and pain medicine fellowship training at UF. After joining the faculty, Dr. Antony served to: grow the fellowship program to national recognition, bring several new procedures to the Florida community, and continue to be a recognized leader in his specialty. Dr. Antony is a member of many professional academic societies such as the Alpha Omega Alpha Honor Medical Society, the North American Neuromodulation Society (NANS), and the International Neuromodulation Society (INS). He has lectured both nationally and internationally and teaches national training courses for fellows and practicing physicians.

About Dr. John Stevenson
Dr. John Stevenson is a board-certified neurosurgeon who specializes in spine surgery, working at The Orthopedic Institute. Dr. Stevenson became a neurosurgeon because of his love for neuroscience and the influence of his father. He received his undergraduate education at Oberlin College and his medical training at the University of Glasgow. He then went on to complete his residency training in neurosurgery at Duke University Medical Center. Dr. Stevenson is a member of numerous professional associations, some of which include The American Association of Neurological Surgeons, Fellow of the Royal College of Surgeons of England, and the Congress of Neurological Surgeons.
Air Date: 10/2/23
Dr. Ajay Antony, a leading interventional pain physician, and Dr. John Stevenson, a renowned neurosurgeon, both affiliated with The Orthopedic Institute in Gainesville, Florida, were recently showcased on the American Society of Pain and Neuroscience’s (ASPN) The Pain Unfiltered Podcast. In medicine today, teamwork between different specialties is revolutionizing care for patients with complex conditions and there is no partnership that exemplifies this better than Dr. Ajay Antony and Dr. John Stevenson.
Join ASPN hosts Dr. Patrick Buchanan and Dr. Timothy Deer as they moderate the conversation around how treatments, like the mild® Procedure, served as a catalyst for discussions that led to deeper understanding and synergy between pain management and surgical intervention.
Key Takeaways:
Listen to the full podcast episode below.
To learn more about how partnerships between interventional pain management and spine surgeons have provided a more comprehensive and effective approach to treating lumbar spinal stenosis (LSS), view our blog article, “Collaborative Care in Spinal Stenosis: Breaking Barriers for Better Patient Outcomes.”
In a recent Pain Medicine News multimedia feature article, Dr. Peter Staats, chief medical officer of the National Spine and Pain Centers, discussed data from his award-winning Top Abstract 2023 at the American Society of Pain and Neuroscience’s (ASPN) 5th annual conference in Miami Beach, FL.
Dr. Staats and his team analyzed a Medicare data set between 2017 and 2019 that included patients who had neurogenic claudication with spinal stenosis and underwent a surgical procedure: either the mild® Procedure or an open laminectomy. They showed that the incidence of harms in the open laminectomy arm was significantly greater compared with the mild® Procedure. Dr. Staats noted, “We all go down the path of trying to treat our patients as conservatively as we can with safety first, and this is clearly demonstrating to be a safer approach.”
In the below video, Dr. Staats discusses his abstract and the conclusions drawn from it. To read more in depth about Staats’ abstract, please visit our blog post, “An Overview of mild® Procedure Abstracts Showcased at the ASPN 2023 Annual Conference.”
Click to Read the Full ArticleTranscript:
(00:00) Hi, I’m Peter Staats. I’m a Pain Medicine advisory board member. I’m also Chief Medical Officer of National Spine and Pain Centers. I’m a long-time Interventional Pain Physician, having been around the space for a little while. I’m thrilled to receive one of the top abstracts at the American Society of Pain and Neuroscience.
(00:32) Our abstract looked at an entire Medicare data set between 2017 and 2019 for patients who had neurogenic claudication with spinal stenosis who had to go up through a surgical procedure, either a mild® Procedure or an open laminectomy.
(00:52) What we showed is that the incidences of harms in the open laminectomy arm was significantly greater. Harms would be things like a wound infection or a dural tear or something that causes the patient some kind of injury.
(01:11) The flip side of that is that there was about a 3-4% increase in the incidence of needing to have a subsequent surgical procedure in the group that underwent the mild® Procedure. So, putting it all together, I think that this starts to really give us a treatment algorithm. We all go down the path of trying to treat our patients as conservatively as we can with safety first, and this is clearly demonstrating to be a safer approach.
(01:40) However, we haven’t lost anything. If the patient doesn’t do well with the mild® Procedure, an open laminectomy is still an option for the patients.
The views and opinions expressed in this article are those of the authors/speakers and do not necessarily reflect the official policy or position of Vertos Medical.
The MOTION Study is designed to measure the impact of percutaneous image-guided lumbar decompression (PILD) as a first-line therapy on patients otherwise receiving real-world conventional medical management for lumbar spinal stenosis (LSS) with neurogenic claudication (NC) secondary to hypertrophic ligamentum flavum.
This Level-1 prospective, multi-center randomized controlled trial uses objective and patient-reported outcome measures to compare the combination of the mild® percutaneous treatment and non-surgical conventional medical management (CMM) to CMM-Alone.
CMM was defined as any conservative or low-risk interventional therapies that are options for early treatment of NC. These options include physical therapy, home exercise, walking aids, early interventional therapies such as epidural steroid injections, lumbar facet medial branch nerve blocks, facet joint injections, and radiofrequency ablation.
Two-year follow-up of the MOTION Study included 64 mild®+CMM and 67 CMM-Alone patients. All outcome measures showed significant improvement from baseline for mild®+CMM, whereas the majority of CMM-Alone patients had elected to receive mild® treatment or other lumbar spine interventions by 2 years, precluding valid 2-year between-group comparisons.
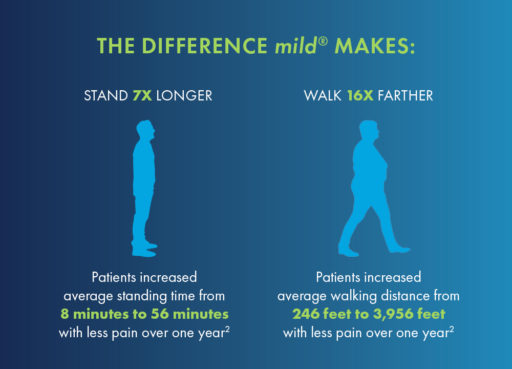
The durability of mild®+CMM for this patient population was demonstrated for all efficacy outcomes through 2 years. Improvements in walking time from baseline to 2 years for patients treated with mild®+CMM were significant and substantial.
Additional 2-year data for patients receiving the mild® Procedure plus CMM include:
Together with subjective patient-reported outcomes, this study demonstrated that the mild® Procedure, when combined with CMM, is superior in providing improved function and decreased pain when compared to CMM-Alone for these patients. CMM can provide some relief for patients only by managing symptoms, while the mild® Procedure instead addresses a primary cause of LSS by debulking the thickened ligamentum flavum and reducing the compression of nerve tissue. The lack of reported device or procedure-related adverse events reinforces the strong safety profile of the mild® Procedure.
These results provide support for early interventional treatment of symptomatic LSS with the mild® Procedure.
Hear from Dr. Timothy Deer, principal investigator for the MOTION Study and Chairman of the American Society of Pain & Neuroscience, as he discusses the 2-year results and why mild® is an effective, early interventional treatment for patients suffering from symptomatic LSS.
Transcript of Dr. Deer’s video:
(00:00):
Hello, I’m Tim Deer. I want to talk to you today about the MOTION Study, a Level-1 study where we have 19 centers in the United States doing real world experiences with a minimally invasive lumbar decompression procedure, mild®. In that study, we have mild® versus medical management, and again, we look at how they do over one and now 24 months. And this is about that publication. You may remember 12 months ago I talked to you about the results of the 12-month publication, and I’m happy to report that the results remain enduring. And what I mean by that, the ODI remains markedly significant. The walking tolerance, which I think is a real measure of lumbar degenerative stenosis treatment, remains excellent. Pain scores remain excellent. All those remain markedly, statistically significantly better in the mild® group. Even more impressively, very few of those patients needed additional surgery for the same condition.
(00:53):
So we really minimized the need for larger, more risky, more expensive procedures, and I think that’s going to be the future of medicine – less invasive, safer for the patient, with really minimal hospitalization stays. The main goal is to continue improving function. The 2-year, 24-month data shows function as markedly better and remains that way. Two years after the procedure, there’s endurance and it’s also in a group of people that really represents the real world. I think what it also shows is medical management alone for stenosis patients, who is trying to avoid a major surgery, doesn’t work very well long term. And I think that’s important to note when we think we’re doing better than we are with our medical management. So, to conclude, real world Level-1 data multicenter, reproducible now, compared to previous studies we’ve done, shows that the therapy of minimally invasive lumbar decompression when the ligamentum flavum is more than 2.5 millimeters causing stenosis, is enduring and has great outcomes. Hope you click on the article below and share the article with your friends. Have a great day.
ALISO VIEJO, Calif., (August 15, 2023) — Vertos Medical Inc., a leader in the development of innovative, minimally invasive treatments for lumbar spinal stenosis (LSS), announced today that its Vice President of Sales, Stephen E. Paul, has been named chief commercial officer (CCO), and its Vice President of Research and Development, Mehrzad Khakpour, Ph.D., has been named chief technology officer (CTO) for the rapidly growing company. The promotions come on the heels of a recent Series C equity funding round of more than $26 million.
Lumbar spinal stenosis impacts one in five Americans over the age of 60. Vertos Medical’s proprietary technology, the mild® Procedure, has been shown in many studies to help restore mobility and decrease pain for LSS patients while greatly improving their quality of life. mild® is an image-guided, outpatient procedure that removes a major root cause of LSS, namely excess ligament tissue in the spinal canal.
“Steve will continue to lead our sales teams and spearhead our commercialization efforts as we work to make mild® the standard of care in medical practices nationwide,” said Eric Wichems, president and CEO of Vertos Medical. “Mehrzad will assume the responsibility of building out our research and development capabilities to expand on the successes of mild® and further develop our product portfolio and intervention options.”
Formerly Vertos’ vice president of sales, Mr. Paul will leverage his more than 20 years of expertise in building and managing high-performance medical device sales and consumer commercial teams. Paul has been responsible for developing and launching multiple market-disrupting products in previous medical device endeavors. In his newly established role, he will oversee marketing, sales, and reimbursement/patient access teams.
Dr. Khakpour, previously Vertos’ vice president of research and development, also boasts more than 20 years of experience in medical device research and innovation, with numerous notable past accomplishments. In his newly created CTO position, he will oversee Vertos’ upstream marketing, R&D, and clinical research teams to steer the company toward promising adjunctive innovations.
Vertos is experiencing a significant increase in demand for its groundbreaking procedure, and more than 75,000 patients have been treated in the United States. The company’s rapid revenue growth of 348% between 2018 and 2021 led Deloitte to rank the company #384 on its prestigious Deloitte Technology Fast 500™ list in November 2022.
“Our future has never been brighter,” says Wichems. “Steve and Mehrzad will continue to grow Vertos’ sales and portfolio to accelerate our commercial expansion and achieve our goal of making the mild® Procedure accessible to every appropriate patient suffering from LSS in the United States.”
About Vertos Medical Inc. and the mild® Procedure
Vertos Medical is an interventional pain company committed to developing innovative, minimally invasive treatments for lumbar spinal stenosis (LSS). mild®, its proprietary technology, is an image-guided outpatient procedure that removes a major root cause of lumbar spinal stenosis (LSS) through an incision smaller than the size of baby aspirin and doesn’t require implants, general anesthesia, or stitches. The mild® Procedure has been clinically demonstrated to have safety outcomes similar to injections with durability out to 5 years, and patients typically return to activities of daily living within 24 hours with no restrictions. mild® is nationally covered by Medicare.
In November 2022, Vertos Medical joined an elite group by ranking 384 on the Deloitte Technology Fast 500™, a ranking of the most innovative, fastest-growing public and private companies from North America. This recognition highlights Vertos Medical’s exceptional growth and relentless pursuit of improving the quality of patients’ lives. Vertos Medical headquarters is located in Aliso Viejo, CA. To learn more and view clinical data, visit www.Vertosmed.com.
View the Full Press ReleaseIn July 2023, the American Society of Pain and Neuroscience (ASPN) held its 5th annual conference in Miami Beach, FL. The society’s goal is to facilitate the role of evidence-based pain medicine research, patient education, and advocacy, and to continue to be on the cutting edge of pain medicine interventions. As part of the conference, a number of abstracts showcased the mild® Procedure, a minimally invasive procedure that debulks thickened ligament in the spinal canal to address a major root cause of lumbar spinal stenosis (LSS). Below are the featured abstracts and their summaries.
Please view the abstracts to review their associated clinical data.
WINNER — Selected as an ASPN Top Abstract 2023
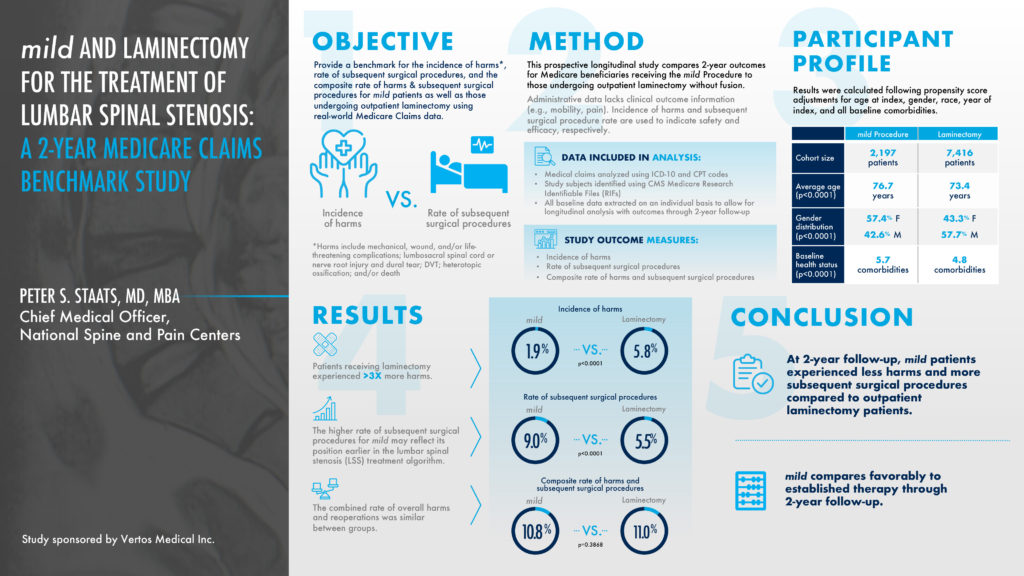
This prospective longitudinal study compared 2-year outcomes for Medicare beneficiaries receiving the mild® Procedure to those undergoing an outpatient laminectomy, a type of spinal surgery. The objective was to provide a benchmark for the incidence of harms versus the rate of subsequent spinal surgical procedures. Patients receiving a laminectomy experienced 3 times more harms at a 5.8% rate, compared to a 1.9% rate for the mild® Procedure. At a 2-year follow-up, mild® patients experienced less harms and more subsequent spinal stenosis surgical procedures compared to outpatient laminectomy patients. The higher rate of subsequent surgical procedures for mild® may reflect its position earlier in the lumbar spinal stenosis treatment algorithm.
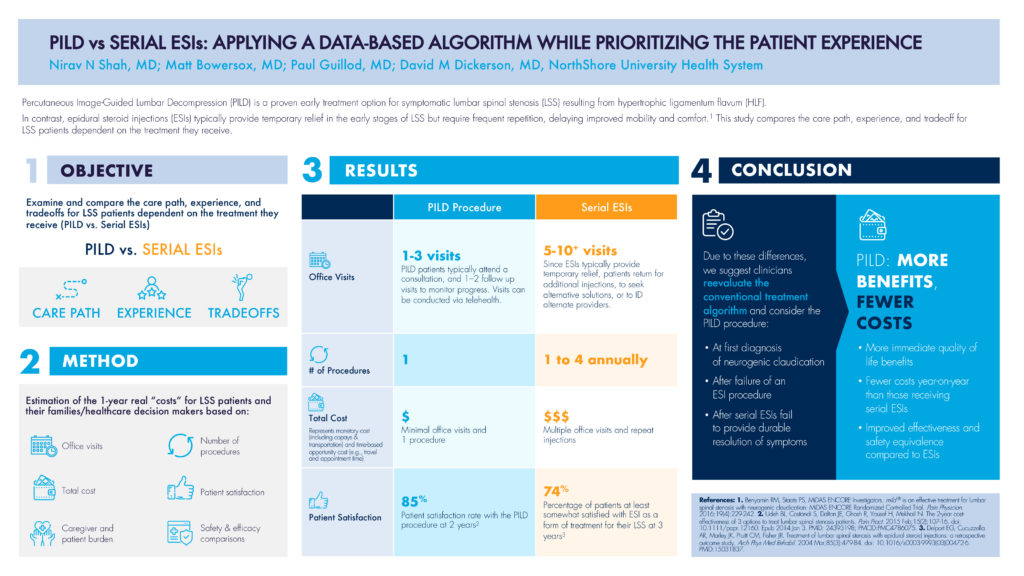
This abstract’s objective was to examine and compare the care path, experience, and tradeoff for LSS patients dependent on the treatment they receive, comparing PILD to serial ESIs (epidural steroid injections). As highlighted in the abstract, Percutaneous Image-Guided Lumbar Decompression (PILD) is a proven early treatment option for symptomatic lumbar spinal stenosis resulting from hypertrophic ligamentum flavum (HLF). In contrast, epidural steroid injections (ESIs) typically provide temporary relief in the early stages of LSS but require frequent repetition, delaying improved mobility and comfort. The methodology estimated the 1-year real “costs” for LSS patients including the number of office visits, the number of procedures, the total cost, and patient satisfaction, to name a few.
In terms of office visits, PILD patients typically attend 1—3 visits including a consultation and follow-up visit, whereas serial ESI patients often return for additional injections, increasing their total number of visits to the 5—10+ range. The total cost of multiple visits shows a three-time multiplier for serial ESI patients compared to PILD patients, where the total cost represents both monetary costs like co-pays and transportation, and the time-based opportunity cost such as travel and appointment time. Even the patient satisfaction rate for PILD patients was 11% higher compared to serial ESI patients, 85%—74%.
Due to these differences, PILD offers more patient-centric benefits and fewer costs, and would be recommended:
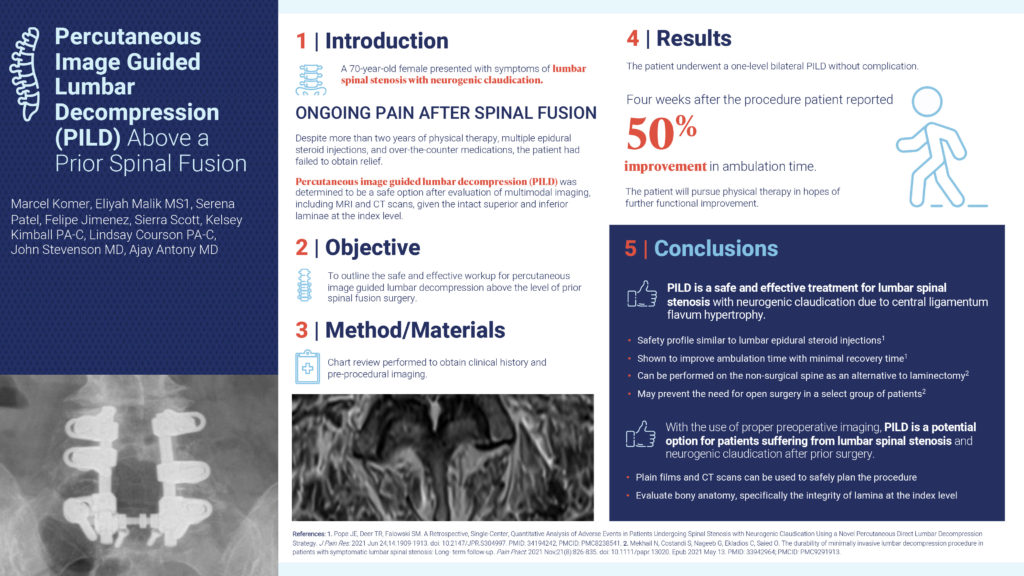
This abstract’s objective was to outline the safe and effective workup for percutaneous image guided lumbar decompression above the level of a prior spinal fusion surgery. In this case study, a 70-year-old female presented with symptoms of lumbar spinal stenosis with neurogenic claudication and felt ongoing pain after a spinal fusion. Despite more than 2 years of physical therapy, multiple epidural steroid injections, and over-the-counter medications, the patient had failed to obtain relief. After an evaluation of MRI and CT scans, the patient underwent a one-level bilateral PILD without complication. Four weeks after the procedure, the patient reported a 50% improvement in ambulation time. In conclusion, with the use of proper preoperative imaging, PILD is a potential option for patients suffering from lumbar spinal stenosis and neurogenic claudication after prior surgery.
This abstract’s objective was to create an approach by which pain practices can increase surgical referrals for PILD by collaborating with surgeon practices, and ultimately optimizing patient care. PILD is an ideal procedure to foster surgeon collaboration since it provides a treatment option for nonsurgical candidates and keeps patient in the practice. Surgical Advanced Practice Providers (APPs) are therefore an ideal PILD referral source as they are familiar with patient histories, have the exposure to nonsurgical candidates, and are eager to optimize patient care. If APPs have knowledge of PILD as a potential treatment, suggesting it as a first option for these nonsurgical patients and collaborating with Interventional Pain Management (IPM) would become routine and enhance patient care.

Authors’ Affiliation
*Novant Spine Specialists, Charlotte, NC, USA
**California University of Science and Medicine, CA, USA
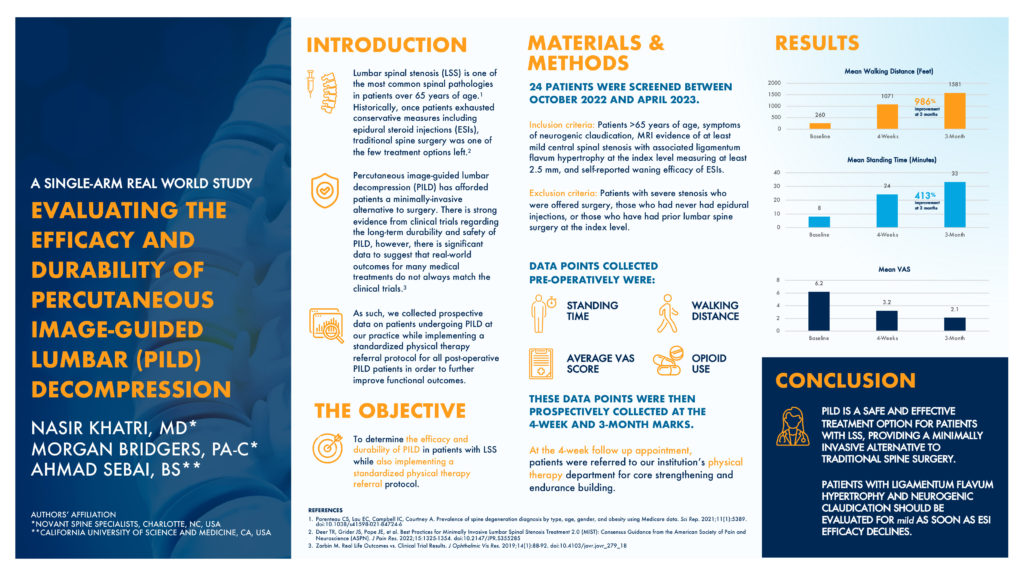
This abstract’s objective was to determine the efficacy and durability of PILD in patients with lumbar spinal stenosis while also implementing a standardized physical therapy referral protocol. These patients were older than 65 years old, with symptoms of neurogenic claudication. They had MRI evidence of at least mild central spinal stenosis with associated ligamentum flavum hypertrophy measuring at least 2.5mm, with a self-reported waning efficacy of epidural steroid injection results. Data points such as standing time and walking distance were collected at a baseline timeframe and 4 weeks post-operatively. At the 4-week follow-up appointment, patients were also referred to a physical therapy routine for core strengthening and endurance building. At the 3-month follow-up, the mean walking distance showed a 986% improvement and the mean standing time showed a 413% improvement. Abstract authors conclude that PILD is a safe and effective treatment option for patients with lumbar spinal stenosis, providing a minimally invasive alternative to traditional spine surgery.
The views and opinions expressed in this article are those of the authors/speakers and do not necessarily reflect the official policy or position of Vertos Medical.
For individuals of any age, mobility is a central wellness indicator that can dramatically impact quality of life. Limited mobility may impact not only physical health and fitness, but also a wide variety of quality-of-life measures, including mental and emotional well-being, social engagement, and access to cultural and recreational experiences.
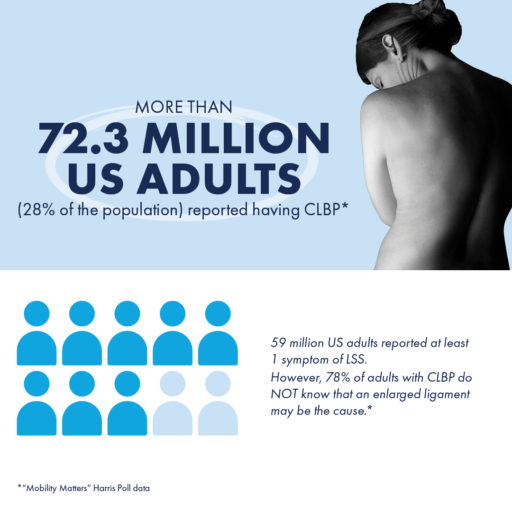
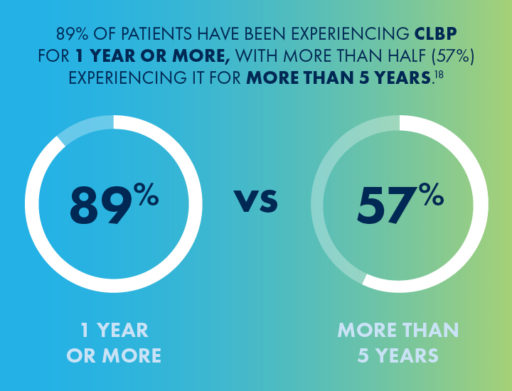
Despite the importance of mobility, large-scale research that demonstrated how limited mobility due to chronic low back pain (CLBP) impacts patients — relative to their non-CLBP peers — did not exist until recently.
To help more patients suffering from CLBP improve their mobility and quality of life, Vertos Medical, in partnership with leaders in interventional pain management, joined forces with The Harris Poll to understand and educate the public about its impact.
Through their groundbreaking work, an entirely new quality-of-life metric, known as the Mobility Index, was developed. This index can help patients suffering from CLBP understand how their mobility compares to others in their age group who do not experience CLBP.
By combining self-reported data on physical abilities, mobility-related statements, and the completion of everyday tasks, the poll results and Mobility Index offer never-before-available perspectives on how extensively CLBP impacts individuals’ quality of life.
On May 11, 2023, Edward “Paul” Johnson, Vice President of Advanced Analytics from The Harris Poll, and Peter Pryzbylkowski, MD, interventional pain specialist, presented an abstract about the poll data and Mobility Index, “Getting America Mobile: Ways to Improve American Quality of Life,” at the 78th annual American Association for Public Opinion Research (AAPOR) conference.
During the session, the presenters outlined 3 primary goals that guided the development of the survey:
To gauge the impact of a range of health conditions on mobility, including chronic low back pain, a survey was conducted across a diverse sample of over 5,000 adults from non-probability, opt-in panels in the United States.
The collected data was carefully weighted by various demographic factors such as age, gender, race/ethnicity, region, education, household income, household size, and marital status to ensure its representativeness according to the 2021 Current Population Survey.
Among the several health conditions investigated, CLBP emerged as the most prominent cause of decreased mobility, even surpassing prevalent conditions such as anxiety, arthritis, and obesity.

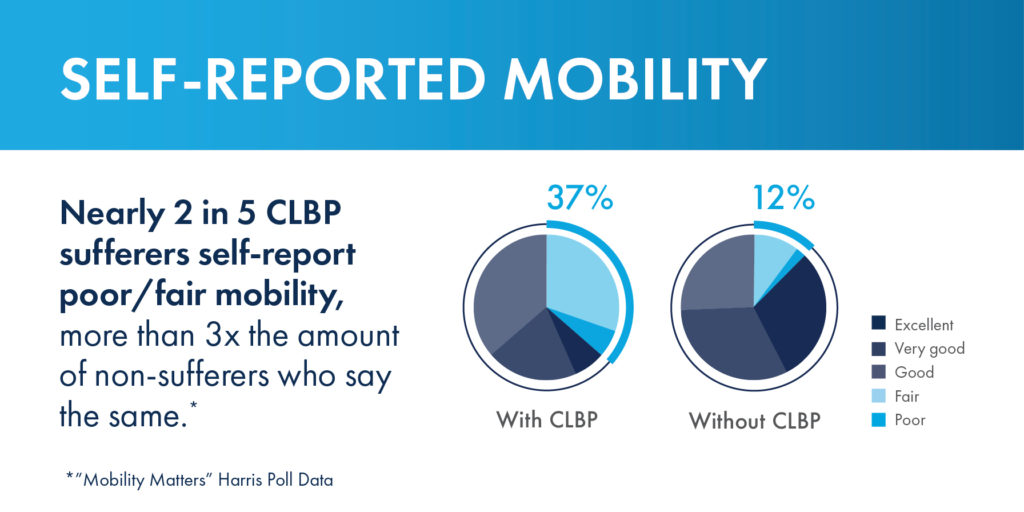
In addition to its utility in measuring mobility and quality of life, the Mobility Index was designed to show patients living with CLBP how they could be moving through the decades of life differently if chronic low back or leg pain was not a limiting factor.
Another concerning disparity revealed in the study was between the prevalence of chronic low back pain and the effectiveness of the most commonly utilized treatment or pain management options.
According to the survey results, up to 15 percent of individuals with CLBP were still relying on opioids , despite updated guidelines from the U.S. Centers for Disease Control (CDC) emphasizing their limited effectiveness and inherent risks.*
Another significant finding was that a mere 5 percent of individuals with CLBP had utilized minimally invasive lumbar decompression treatment options such as the mild® Procedure, despite research indicating that these procedures are highly effective and should be considered earlier in the treatment process.
See More Findings From the Survey
The findings of the Mobility Matters survey were instrumental not only in the development of the Mobility Index but in starting a national public health conversation that spreads awareness about the impacts of CLBP and quality of life.
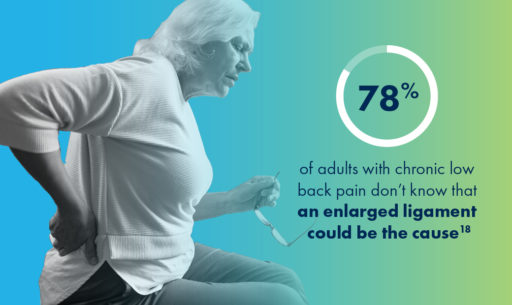
According to the survey, physicians appear to discuss osteoarthritis or aging as potential causes of CLBP more often than lumbar spinal stenosis, particularly the enlarged ligament that can cause LSS.
By raising awareness about LSS among providers and providing education on the treatment options available for patients suffering from the condition, more patients could get on the path to lasting relief sooner.
“What we found [through the survey] was that CLBP was really a limiting factor when it came to the ability for patients to walk and stand for a prolonged period of time,” Dr. Pryzbylkowski said.
“And that’s important because there are board-certified physicians like myself who treat chronic low back pain on a daily basis. And we just want to bring education and awareness to the general public that there are treatment options for CLBP.”
Through the insights gathered in the Mobility Matters survey, patients, healthcare providers, and policymakers can all gain greater knowledge about the effectiveness of alternative treatment options, the risks associated with opioid use, and the importance of early intervention for CLBP.
Learn more about the Mobility Index and Mobility Matters survey at:
References
*Centers for Disease Control and Prevention. Acute low back pain. https://www.cdc.gov/acute-pain/low-back-pain/index.html. Accessed July 21, 2022.
Over 2 million people are diagnosed with lumbar spinal stenosis annually. Spinal stenosis usually presents with lower back pain when standing up straight, an aching sensation, numbness, and tingling and pain in buttocks when patients are walking. Dr. Rayhan Tariq, Interventional Pain Management physician, offers an alternative to open spine surgery known as mild® — minimally invasive lumbar decompression.

Deborah Butler’s pain was at a level 9 by the time she found help at South Central Pain Center. Mrs. Butler said, “I woke up and my hip, all the way down to my knee, was in horrible pain.” After meeting with various physicians and trying physical therapy, Mrs. Butler contacted Dr. Tariq to discuss alternative treatments. Together, they made the decision to perform the mild® Procedure on Mrs. Butler. Today, she states, “My pain level has decreased to a level 2, and I have regained my quality of life.”
View Full Article & Video
The views and opinions expressed in this article are those of the authors/speakers and do not necessarily reflect the official policy or position of Vertos Medical.
Original Publish Date: Jan 19, 2023
Contributing Writer for Novant Health: Page Leggett
Article Excerpts:
Sherry Clayton, 74, has always been active. Like many people her age, she had arthritis—but it didn’t keep her from doing the things she loved. Then, in June 2021, her pain became too much. An MRI revealed that she had lumbar spinal stenosis, a disease that occurs when the space inside the spine becomes too small, placing pressure on the spinal cord and nerve roots.
The condition is more common in older populations. One out of every 1,000 people over the age of 65 is likely to develop spinal stenosis, according to the National Institutes of Health (NIH).
Clayton, a resident of Fort Mill, South Carolina, saw two spine surgeons, both of whom recommended spinal fusion surgery—but even that wouldn’t guarantee she’d be pain-free. Not being one to accept the status quo, Clayton did some research. She found the website for Vertos Medical and liked what she read about the minimally invasive lumbar decompression, mild® Procedure, which led her to Dr. Nasir Khatri. He and his partner, Dr. Jacob Wang, are two of just a handful of doctors in the Charlotte area trained on the procedure. Vertos is a medical device company that manufactures the specialized equipment necessary to perform the procedure.
About six weeks after her initial consultation with Khatri, Clayton went to Novant Health Presbyterian Medical Center—the very hospital where she was born—to have the same-day procedure. Khatri reported: “At her two-week follow-up appointment, she reported having nearly 75% pain relief and, more importantly, improved function. Based on her Apple Watch data, she is now walking double the steps she could before.”
Click to Read the Full ArticleThe views and opinions expressed in this article are those of the authors/speakers and do not necessarily reflect the official policy or position of Vertos Medical.
Congratulations to Nicole Arnold, our Director of Human Resources,  who was recently recognized as one of the Orange County Business Journal’s Distinguished Leaders: Human Resources 2023. The annual list honors HR leaders who have navigated the ever-changing HR landscape and demonstrated an impact within their organization and the Orange County community.
who was recently recognized as one of the Orange County Business Journal’s Distinguished Leaders: Human Resources 2023. The annual list honors HR leaders who have navigated the ever-changing HR landscape and demonstrated an impact within their organization and the Orange County community.
Nicole Arnold has brought significant improvements to our organization’s performance during her tenure. She has implemented various initiatives to strengthen our team and keep morale in check. Firstly, she led the extraction of a comprehensive People Experience Organization (PEO) for HR functions and onboarding to our own Human Capital Management system, all while building the HR team and functions from bottom up. Furthermore, she ensured that our employees were always at the forefront of every decision, offering strategic advice and advocating employee benefits, while also finding ways of streamlining processes and improving morale. We are grateful for her dedication and contributions.
Read the Full PublicationVertos Medical is proud to have joined forces with the American Society of Pain & Neuroscience (ASPN) and the National Association of Memoir Writers (NAMW) to develop the Know Your Back Story campaign, a national public health awareness campaign that seeks to help patients suffering from chronic low back pain (CLBP) learn more about their “back stories.” The campaign encourages providers to educate their patients on lumbar spinal stenosis (LSS) and provide awareness around the enlarged ligament that may be causing their pain.
Vertos Medical is committed to empowering healthcare providers and patients with minimally invasive treatments for LSS, and the Know Your Back Story campaign plays a significant role in fulfilling our core mission: to help patients suffering from chronic back pain reclaim their quality of life using the simplest, safest, most durable, and earliest treatment available.
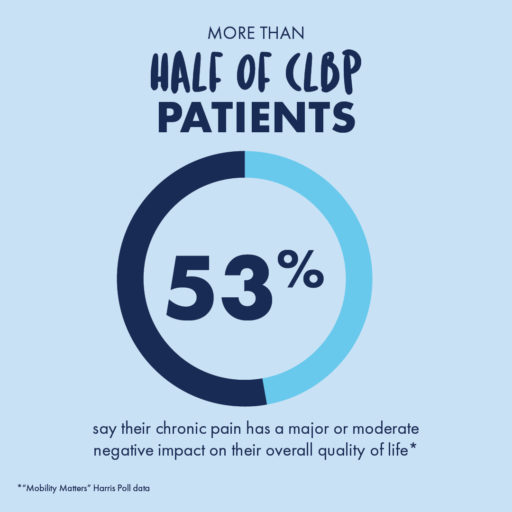
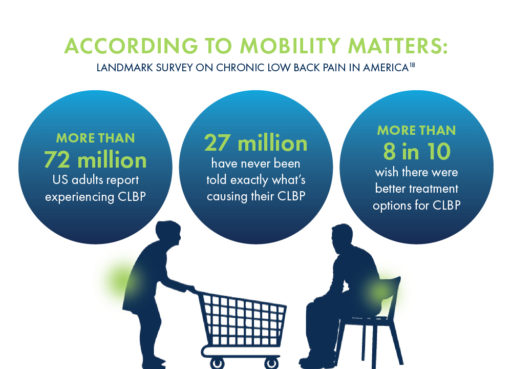
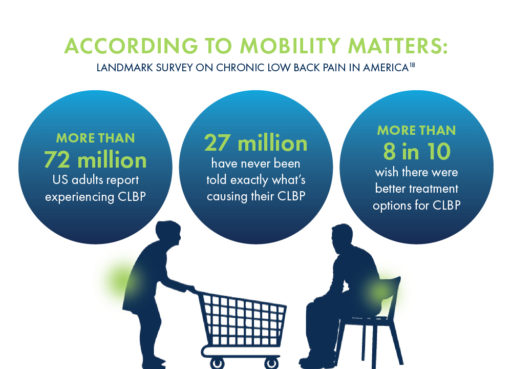
As part of the Know Your Back Story campaign, we partnered with The Harris Poll to conduct a landmark survey on CLBP in the United States. Results from the “Mobility Matters: Chronic Low Back Pain in America” survey indicate that CLBP affects more people than arthritis, diabetes, or heart disease, but over one-third of CLBP patients have never been told by a provider what the exact cause of their pain is.
“Mobility Matters: Landmark Survey on Chronic Low Back Pain in America” also revealed misconceptions about CLBP and the need for education about the associated impacts on mobility and quality of life, and where to go to for diagnoses and information about available treatment options.
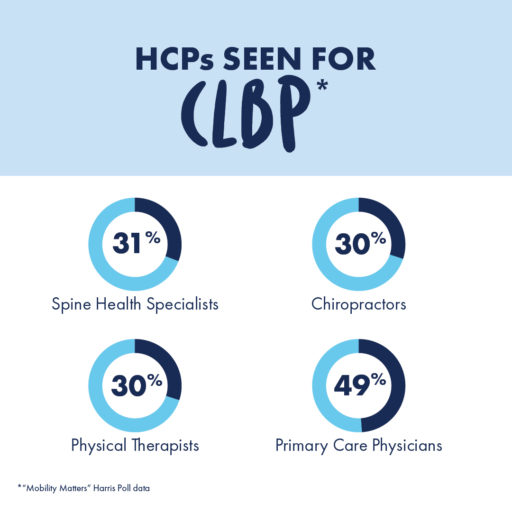
The average chronic low back pain sufferer has seen at least 3 different healthcare professionals (HCPs) seeking treatment for their pain and has made 4 visits to an HCP within the last year.
For the most accurate diagnoses and treatment recommendations that may lead to lasting relief, patients should seek out doctors who specialize in spine health, such as pain specialists, physical medicine, and rehabilitation (PM&R) physicians, interventional pain physicians, or physiatrists.
By meeting with doctors who specialize in spine health, patients may be able to gain new insights into the root cause of their pain.
Lumbar spinal stenosis (LSS) is a condition, prevalent in approximately 20% of patients over the age of 60, in which the lower spinal canal narrows and compresses the nerves in the lower back. Up to 85% of spinal canal narrowing is caused by an enlarged ligament.
This pressure around the spinal cord can cause pain, numbness, heaviness, or tingling in the low back, legs, and buttocks, but the vast majority of CLBP patients have never heard of this potential diagnosis.
The Know Your Back Story campaign’s objective is to spread awareness around LSS and get more patients on the path to lasting relief. By collecting intensive data, developing tools for patient education, and sharing insights with both patients and providers about the effects of LSS and its potential treatment options, the Know Your Back Story campaign has served as a significant step in bringing more visibility to this condition.
Getting screened for LSS and CLBP can open the door to learning more about treatment options available, such as the mild® Procedure.
One of the key accomplishments of the Know Your Back Story campaign is the development of the first-ever Mobility Index, a breakthrough resource for demonstrating the differences in mobility and quality of life between patients with CLBP and their peers without CLBP.
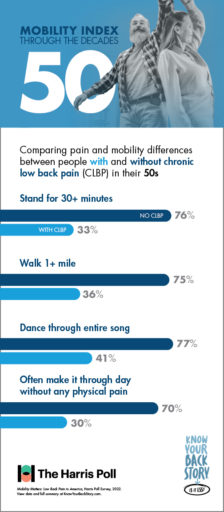
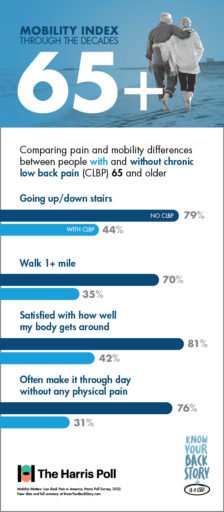
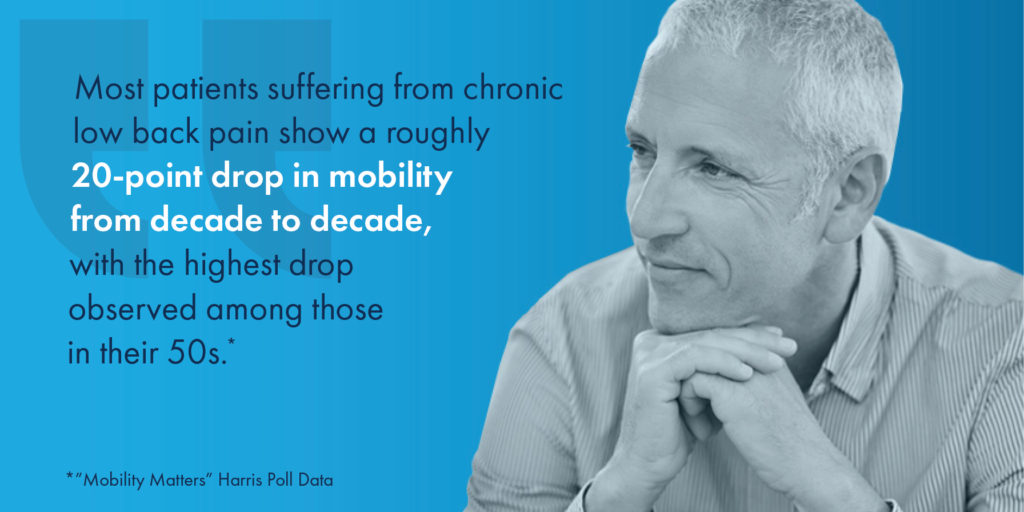
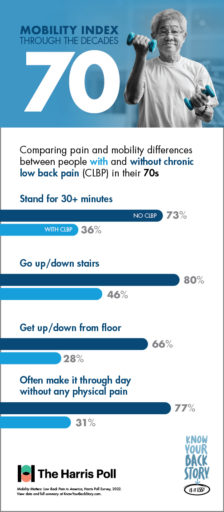
Results from the “Mobility Matters: Landmark Survey on Chronic Low Back Pain in America” conducted by The Harris Poll show that with age, CLBP patients experience significantly greater challenges performing physical tasks and making it through the day without pain or limited mobility than others within their age group without low back pain.
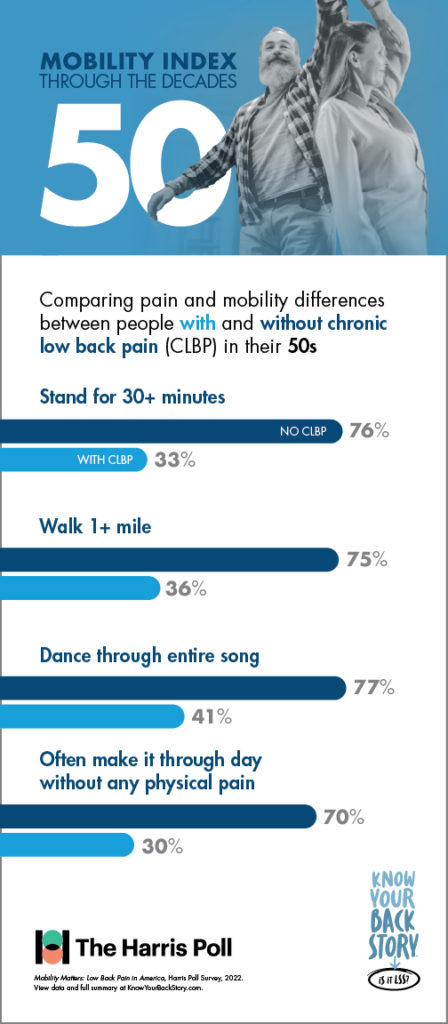
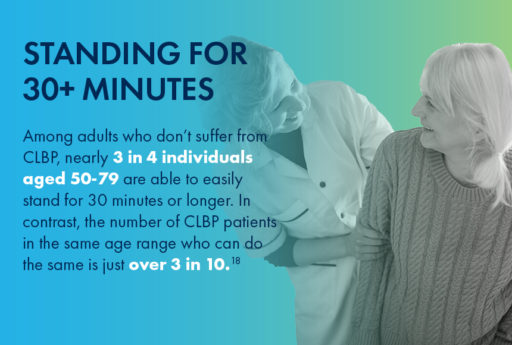
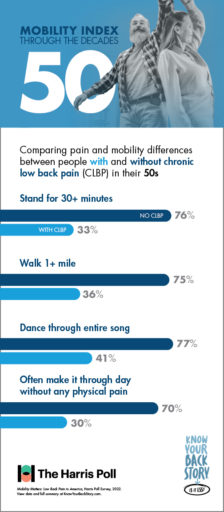
For instance, nearly 3 in 4 individuals in their 50s who do not suffer from CLBP are able to easily stand for half an hour or longer. In contrast, the number of CLBP patients in the same age range who are able to do the same is just over 3 in 10.
When it comes to other activities such as walking, dancing, or using the stairs, the Mobility Index can be a great tool for educating patients. By reviewing the differences in mobility between similar individuals with and without CLBP, patients can understand more about what chronic pain is keeping them from—and their options for finding lasting relief.
On the quest to educate, engage, and increase awareness within communities, the Know Your Back Story campaign took the #LookForTheLigament Education and Experiential Mobile Unit on tour down the East Coast, stopping in New York City, NY; Philadelphia, PA; Washington, D.C.; and Sarasota, West Palm Beach, and Miami, FL.
The mission of this tour was to encourage people suffering from CLBP to get screened for LSS and an enlarged ligament by a spine health doctor, and to provide both patients and HCPs with an in-depth look at the causes and effects of LSS through interactive experiences and demonstrations, including:
By staying aware of the impacts of LSS and CLBP on patients’ mobility and potential treatment options, healthcare providers can help more patients in their communities get on the path to lasting relief. By working alongside others in their practice or by creating referral networks with primary care, physical therapy providers, and other local providers, HCPs in Interventional Pain Management (IPM) or spine health specialties can play a more effective role in identifying patients suffering with LSS or CLBP and connect them to providers that are able to offer more durable treatment options.
Physicians and Advanced Practice Providers (APPs) can also play a more proactive role in identifying LSS by staying aware of common patient misconceptions about back pain. By utilizing the tools and resources developed as part of the Know Your Back Story campaign, you can keep your patients as educated as possible about the potential causes of their chronic pain, as well as the treatment options that may finally provide them with relief.
For patients looking to learn more about the source of their pain and their options for relief, finding a local spine health doctor is a crucial first step. By using the MD Finder tool, patients can find doctors in their area who may be able to provide the answers they’ve been seeking.
A spine health specialist can help walk patients through their options for treatment, from more conservative therapies such as medication or physical therapy to longer lasting, minimally invasive treatments such as the mild® Procedure.
The mild® Procedure, or minimally invasive lumbar decompression, may be pursued as a first-line therapy for LSS.
A minimally invasive procedure that is considered the gold standard of care in LSS treatment, mild® addresses a major root cause of LSS by debulking the enlarged ligament to restore space in the spinal canal and reduce compression of the nerves. With a safety profile equivalent to an epidural steroid injection (ESI), mild® has helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief,—a durable, lower-risk treatment option to spacer implants or open surgery.

For patients considering mild®, the Move More Questionnaire is a great resource for identifying current limitations and tracking their reduced pain and improved mobility after the procedure.
By becoming familiar with the Know Your Back Story campaign and exploring the insights and resources developed to spread awareness about LSS, both patients and providers can help spread the word about this under-diagnosed cause of CLBP.
Vertos Medical is committed to helping patients experiencing chronic pain reclaim their quality of life with a short, minimally invasive early treatment option with the mild® Procedure, both through the Know Your Back Story campaign and in everything we do.

We’re proud to highlight Ashley Comer, A.P.R.N., NP-C, on her educational Op-Ed article in the Charleston Gazette! As a member of our Advanced Practice Provider (APP) Advisory Board and as a nurse practitioner working within Interventional Pain Management (IPM), Ashley interacts daily with patients suffering from chronic low back pain (CLBP), many of whom are simply searching for relief.
Data from a recent Harris Poll survey found that nearly 3 out of every 10 US adults currently suffer from CLBP, and over a third of those surveyed rated their back pain as “severe.” Many of these individuals visited multiple doctors, and while their pain progressed, only then considered seeing an Interventional Pain Specialist.
Read Ashley’s insights below on why patients should consider IPM at the onset of pain treatment and potential treatment options outside of the often-prescribed opioids.
View Full Publication
BCBS Federal Employee Program Medical Policy
TRICARE, Tricare for Life Medical Policy
mild® Medicare Advantage Prior Authorization Request Template
mild® Commercial Prior Authorization and Pre-Determination Template
mild® Prior Authorization or Claim Denial Appeal Template
mild® Procedure Description and Clinical Evidence & FDA Clearance
mild® Medicare Peer-to-Peer Review Guide
For Coding, Coverage and Reimbursement support, click here.
If you experience chronic low back pain (CLBP), you may have questions: What’s causing it? What do my symptoms mean? Will my condition worsen as I age? How can I find relief?
You’re looking for answers—and you’re not alone. Unlike other debilitating conditions, researchers have never truly known how many people suffer from CLBP. Until recently, many patients have been left in the dark about the cause of their pain or their options for treatment.
As revealed in the Mobility Matters: Landmark Survey on Chronic Low Back Pain in America, created in partnership with The Harris Poll, there are many misconceptions about chronic low back pain, including its potential causes, symptoms, and treatment options.
Before this survey, we didn’t know which patients were suffering the most, or how the CLBP experience may change through life’s decades. In this blog, we’ll share the results of the survey, explore a common, yet often undiagnosed, cause of CLBP, and discuss some of the treatment options available for patients seeking relief.
As we grow older, it can be difficult to assess which mobility challenges are a normal part of aging, and which ones may indicate a condition such as CLBP. The Mobility Index, developed as part of the national Know Your Back Story campaign, was designed to demonstrate how older adults could be moving through life if chronic low back or leg pain was not a limiting factor.
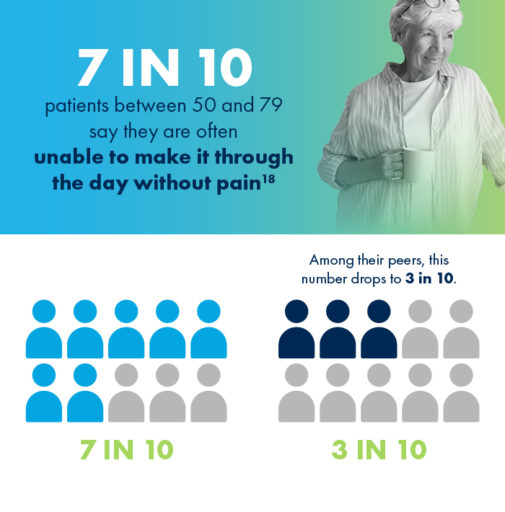
Poll results show that with age, CLBP patients experience significantly greater challenges performing physical tasks and making it through the day without pain than their peers who do not suffer from low back pain.
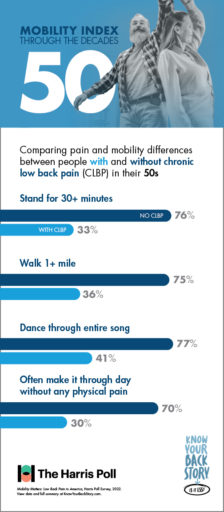
If you’re suffering from CLBP, you’re already familiar with the limits your pain can put on daily tasks and activities. But do you know just how much you could be doing without these obstacles?
For CLBP patients in their 50s, having difficulty doing physical activities that were once a regular part of life, such as walking a mile or dancing for the duration of one song, can feel especially discouraging.

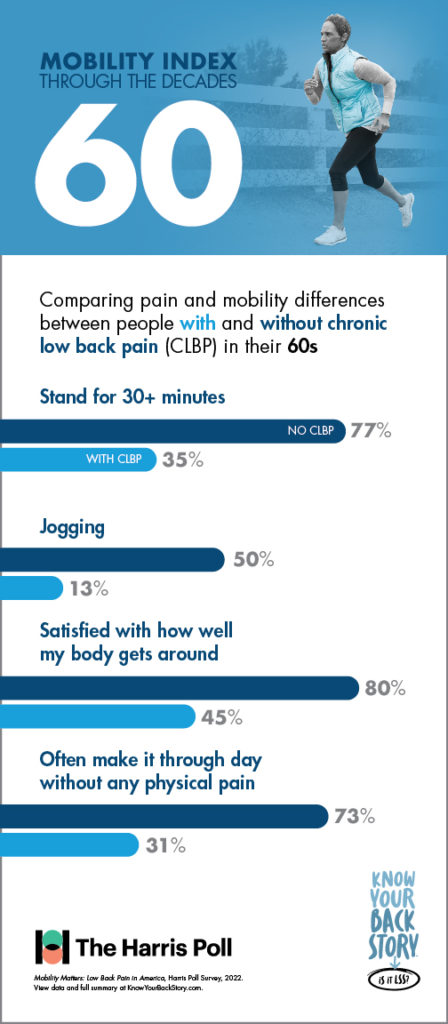
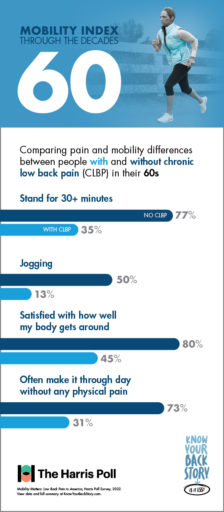
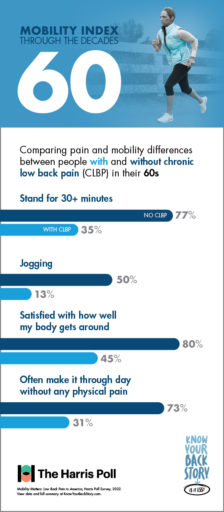
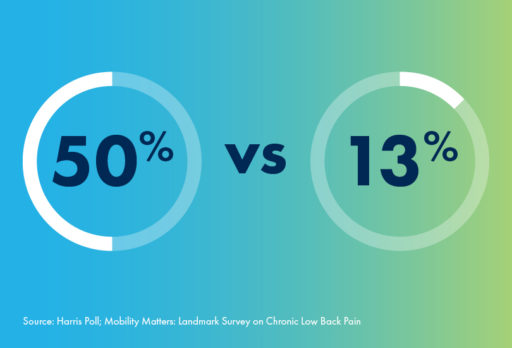
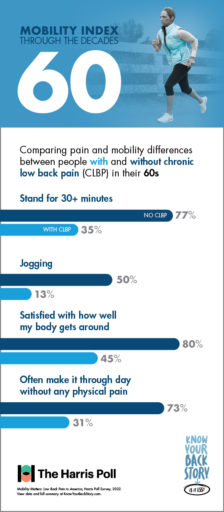
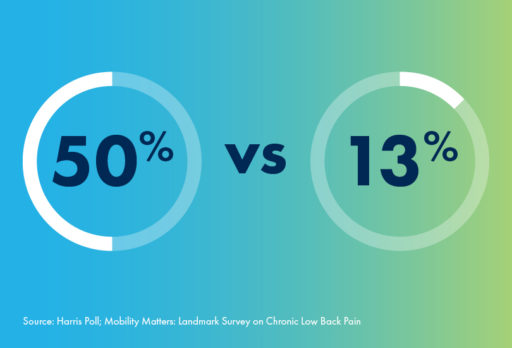
For people in their 60s, there are some activities like—jogging—that aren’t for everyone. Even among individuals without CLBP, only 50% of respondents in their 60s reported the ability to jog with ease. However, for patients suffering with chronic low back pain, this number plummets to only 13%.
And whether jogging, walking, or doing anything else, fewer than half of CLBP patients in their 60s say they feel satisfied with how their body gets around. In contrast, 80% of 60-somethings without CLBP are satisfied with their mobility.
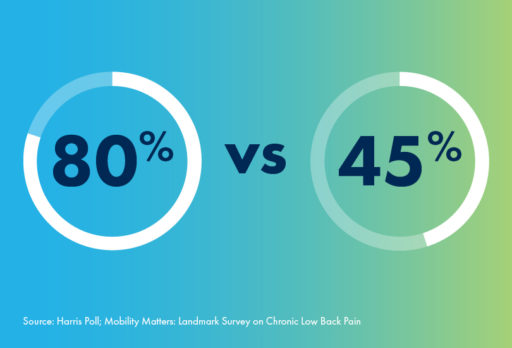
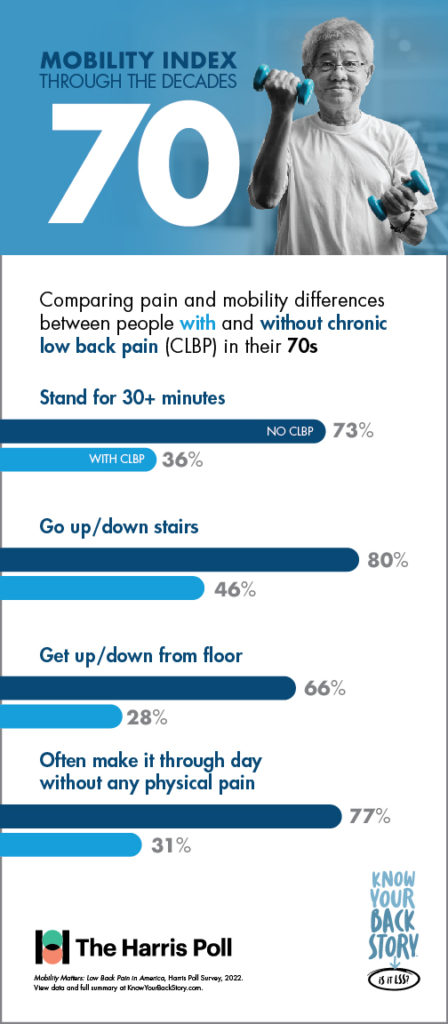
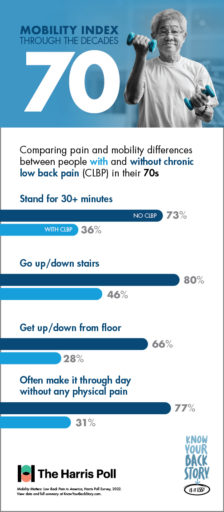
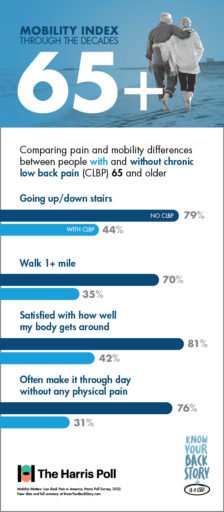
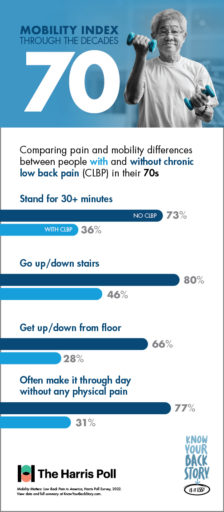
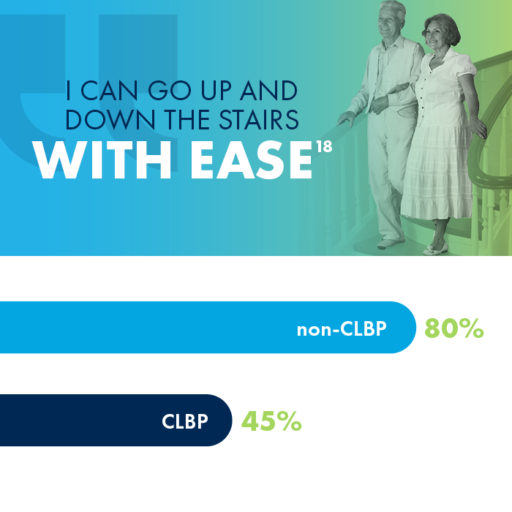
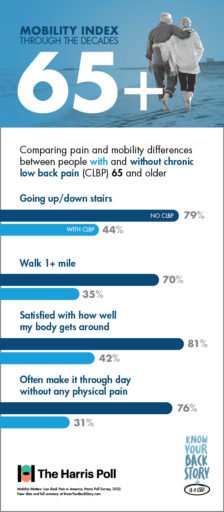
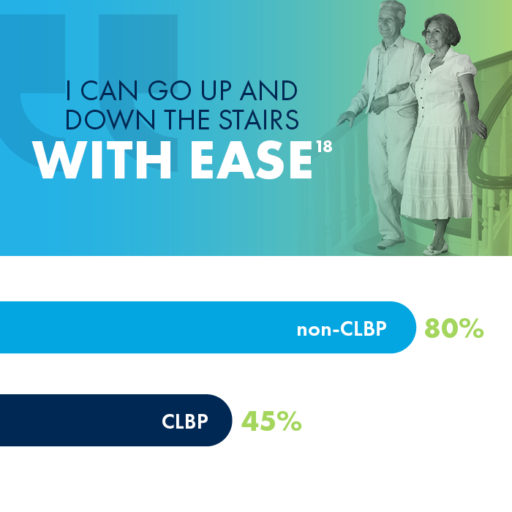
Did you know that 80% of people in their 70s without CLBP are able to easily go up and down the stairs? If you are a CLBP sufferer in your 70s, you may have a much different experience, as fewer than half of CLBP patients in their 70s reported the same mobility using stairs.
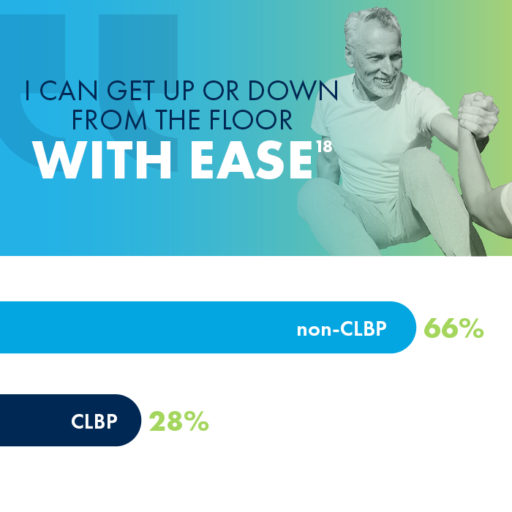
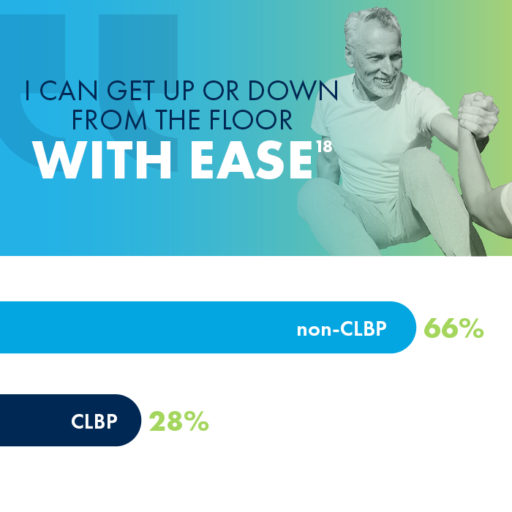
Getting up from the floor is another activity that impacts CLBP sufferers much more than their peers who don’t experience chronic pain. While 66% of 70-somethings without CLBP reported ease in getting up or down from the floor, only 28% of those with CLBP were able to say the same.

One cause of low back pain that often goes undiagnosed is an enlarged ligament, which can contribute to lumbar spinal stenosis (LSS), a common, yet overlooked, condition that millions of people may be unaware of.
Lumbar spinal stenosis (LSS) is a common, yet overlooked, condition that is prevalent in nearly 20% of patients over the age of 60.
LSS is often caused by an enlarged ligament in the back, which compresses the space in the spinal canal and puts pressure on the nerves in the lower back. This pressure around the spinal cord can cause pain, numbness, heaviness, or tingling in the low back, legs, and buttocks.
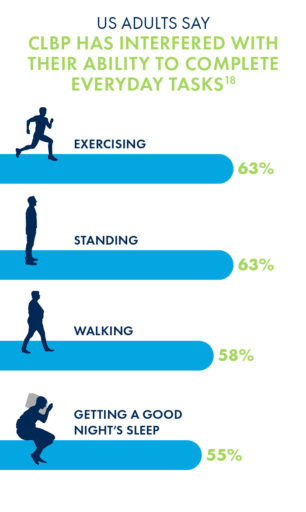
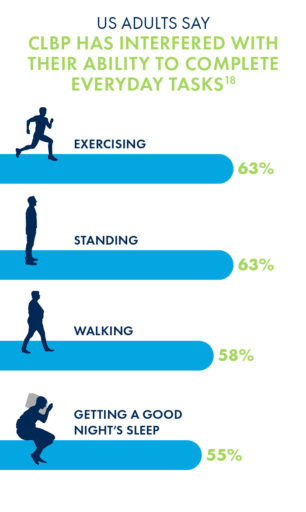
Unsurprisingly, the chronic low back pain that may be caused by LSS has negative impacts on nearly every aspect of a patient’s life, most commonly in their abilities to exercise, stand or walk for long periods of time, and get a good night’s sleep.
Due to its minimally invasive nature and long-lasting durability, many interventional pain management doctors are making the move to mild® as an alternative to epidural steroid injections (ESIs), which may only work in the short-term and may require repeat injections to maintain relief.
More invasive courses of treatment can include procedures such as spacer implants or open surgery, though nearly 80% of CLBP sufferers have concerns about undergoing surgery.
The mild® Procedure, or minimally invasive lumbar decompression, is considered a gold standard of care among treatments for low back pain. By addressing the root cause of pain, the enlarged ligament, mild® has helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief.
When patients present complaining of chronic low back pain (CLBP), they’re relying on you, as their provider, to help them find answers. Many patients want to know what’s causing their pain, how their condition will progress over time, and perhaps most importantly, how they can find relief.
As revealed in the Mobility Matters: Landmark Survey on Chronic Low Back Pain in America, created in partnership with The Harris Poll, many CLBP patients feel that they have been left in the dark about the cause of their pain or their options for treatment; as a provider, you’re all too familiar with the challenges and frustrations that can come with chronic pain.
In this blog, we’ll share some of the results of the groundbreaking survey, including new insights into how CLBP can impact patients’ lives as they age. We’ll also explore a common, though often undiagnosed, cause of CLBP and discuss some of the treatment options available for patients seeking relief.
By staying informed about the causes of low back pain, educating patients about their treatment options, and encouraging patients to seek help from spine health specialists, healthcare providers can play a key role in improving patients’ quality of life.
One cause of CLBP that often goes undiagnosed is an enlarged ligament in the lower back, which can contribute to lumbar spinal stenosis (LSS). LSS is a common, yet overlooked, condition that is prevalent in nearly 20% of patients over the age of 60.
LSS is often caused by an enlarged ligament in the back, which compresses the space in the spinal canal and puts pressure on the nerves in the lower back. This pressure around the spinal cord can cause pain, numbness, heaviness, or tingling in the low back, legs, and buttocks.
By recognizing the symptoms and understanding the treatment options, you may be able to identify the condition sooner in your patients with chronic low back pain and get them on the path to lasting relief.

Unsurprisingly, CLBP that may be caused by LSS has negative impacts on nearly every aspect of a patient’s life—most commonly in the ability to exercise, stand or walk for long periods of time, or get a good night’s sleep.
As patients age, it can be difficult to assess which mobility challenges are a normal part of aging, and which may have an explanation, such as an enlarged ligament.
The Mobility Index was designed to demonstrate just how different life could be for older adults if chronic low back or leg pain was not a limiting factor.
Results from the Mobility Matters survey indicate that adults with CLBP face significantly more difficulties performing physical activity and making it through the day without pain than their peers without chronic pain.
Patients who suffer from CLBP are already familiar with the limits their pain can put on carrying out daily tasks and activities. But they may not even realize just how much they’re missing out.
When it comes to activities such as walking, dancing, using the stairs, and more, the Mobility Index can be a great tool for educating patients. By reviewing the differences in mobility between individuals with and without CLBP, you can help your patients understand more about their mobility and their options for relief.
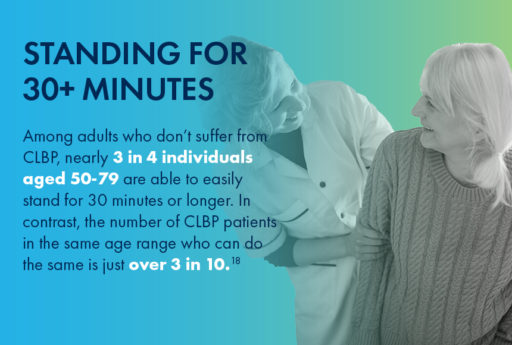
For CLBP patients in their 50s, having difficulty doing physical activities that were once a regular part of life, such as walking a mile or dancing for the duration of one song, can feel especially discouraging.

For patients in their 60s, there are some activities—like jogging—that aren’t especially popular. Even among individuals without CLBP, only 50% of respondents in their 60s reported the ability to jog easily. However, for patients suffering with CLBP, this number plummets to only 13%.

80% of people in their 70s without CLBP are able to easily go up and down the stairs. But the experience may be significantly more challenging for CLBP patients of the same range, as fewer than half of those with CLBP were able to say the same.
Getting up from the floor is another activity that impacts CLBP sufferers much more than their peers who don’t experience chronic pain. While 66% of 70-somethings without CLBP reported ease in getting up or down from the floor, only 28% of those with CLBP were able to say the same.
If you think lumbar spinal stenosis could be causing a patient’s low back pain, and common conservative treatment options such as physical therapy, pain medication, and epidural steroid injections (ESIs) are no longer providing adequate relief, it may be time to move to mild®.
The mild® Procedure, or minimally invasive lumbar decompression, is considered a gold standard of care among treatments for lumbar spinal stenosis. By addressing the root cause of pain, the enlarged ligament, mild® has helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief.
Due to its minimally invasive nature and long-lasting durability, many interventional pain management physicians are making the move to mild® as an alternative to epidural steroid injections (ESIs), which may only work short-term and may require repeat injections to maintain relief.
More invasive courses of treatment can include procedures such as spacer implants or open surgery, though nearly 80% of CLBP sufferers have concerns about undergoing surgery.
For patients experiencing chronic low back pain, it’s never too early to act. Without addressing the root cause of pain—such as the enlarged ligament in cases of LSS—patients can often go years without finding relief.
The Know Your Back Story campaign, a national public health awareness campaign, educates and encourages millions of people with CLBP to learn more about their “back story” and encourages providers to educate patients about LSS and the enlarged ligament that may be the source of this pain.
If your patients are seeking answers for chronic low back pain, they may benefit from the mild® Procedure as a first course of treatment. By referring patients to a local interventional pain management physician, you can help get them on the path to lasting relief.
Access more resources about the Know Your Back Story Campaign and the Mobility Matters Poll
Benyamin RM, Staats PS, MiDAS ENCORE Investigators. mild® is an effective treatment for lumbar spinal stenosis with neurogenic claudication: MiDAS ENCORE Randomized Controlled Trial. Pain Physician. 2016;19(4):229-242.
Mekhail N, Costandi S, Abraham B, Samuel SW. Functional and patient-reported outcomes in symptomatic lumbar spinal stenosis following percutaneous decompression. Pain Pract. 2012;12(6):417-425. doi:10.1111/j.1533-2500.2012.00565.x.
2012 data from Health Market Sciences report for Vertos Medical 2013.
Data on file with Vertos Medical.
Staats PS, Chafin TB, Golvac S, et al. Long-term safety and efficacy of minimally invasive lumbar decompression procedure for the treatment of lumbar spinal stenosis with neurogenic claudication: 2-year results of MiDAS ENCORE. Reg Anesth Pain Med. 2018;43:789-794. doi:10.1097/AAP.0000000000000868.
Based on mild® Procedure data collected in all clinical studies. Major complications are defined as dural tear and blood loss requiring transfusion.
MiDAS ENCORE responder data. On file with Vertos Medical.
Jain S, Deer TR, Sayed D, et al. Minimally invasive lumbar decompression: a review of indications, techniques, efficacy and safety. Pain Manag. 2020;10(5). https://doi.org/10.2217/pmt-2020-0037. Accessed June 1, 2020.
Deer TR, Grider JS, Pope JE, et al. The MIST Guidelines: the Lumbar Spinal Stenosis Consensus Group guidelines for minimally invasive spine treatment. Pain Pract. 2019;19(3)250-274. doi:10.1111/papr.12744.
Hansson T, Suzuki N, Hebelka H, Gaulitz A. The narrowing of the lumbar spinal canal during loaded MRI: the effects of the disc and ligamentum flavum. Eur Spine J. 2009;18(5):679-686. doi:10.1007/s00586-009-0919-7.
Treatment options shown are commonly offered once conservative therapies (e.g., physical therapy, pain medications, chiropractic) are not providing adequate relief. This is not intended to be a complete list of all treatments available. Doctors typically recommend treatments based on their safety profile, typically prioritizing low risk/less aggressive procedures before higher risk/more aggressive procedures, but will determine which treatments are appropriate for their patients.
The mild® Procedure is a minimally invasive treatment for lumbar spinal stenosis. As with most surgical procedures, serious adverse events, some of which can be fatal, can occur, including heart attack, cardiac arrest (heart stops beating), stroke, and embolism (blood or fat that migrates to the lungs or heart). Other risks include infection and bleeding, spinal cord and nerve injury that can, in rare instances, cause paralysis. This procedure is not for everyone. Physicians should discuss potential risks with patients. For complete information regarding indications for use, warnings, precautions, and methods of use, please reference the devices’ Instructions for Use.
Patient stories on this website reflect the results experienced by individuals who have undergone the mild® Procedure. Patients are not compensated for their testimonial. The mild® Procedure is intended to treat lumbar spinal stenosis (LSS) caused by ligamentum flavum hypertrophy. Although patients may experience relief from the procedure, individual results may vary. Individuals may have symptoms persist or evolve or other conditions that require ongoing medication or additional treatments. Please consult with your doctor to determine if this procedure is right for you.
Reimbursement, especially coding, is dynamic and changes every year. Laws and regulations involving reimbursement are also complex and change frequently. Providers are responsible for determining medical necessity and reporting the codes that accurately describe the work that is done and the products and procedures that are furnished to patients. For this reason, Vertos Medical strongly recommends that you consult with your payers, your specialty society, or the AMA CPT regarding coding, coverage and payment.
Vertos Medical cannot guarantee coding, coverage, or payment for products or procedures. View our Billing Guide.
Vertos is an equal employment opportunity workplace committed to pursuing and hiring a diverse workforce. We strive to grow our team with highly skilled people who share our culture and values. All qualified applicants will receive consideration for employment without regard to sex, age, color, race, religion, marital status, national origin, ancestry, sexual orientation, gender identity, physical & mental disability, medical condition, genetic information, veteran status, or any other basis protected by federal, state or local law.
Hall S, Bartleson JD, Onofrio BM, Baker HL Jr, Okazaki H, O’Duffy JD. Lumbar spinal stenosis. Clinical features, diagnostic procedures, and results of surgical treatment in 68 patients. Ann Intern Med. 1985;103(2):271-275. doi:10.7326/0003-4819-103-2-271.
Kalichman L, Cole R, Kim DH, et al. Spinal stenosis prevalence & association with symptoms: The Framingham Study. Spine J. 2009;9(7):545-550. doi:10.1016/j.spinee.2009.03.005.
Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998;14(2):148-151. doi:10.1097/00002508-199806000-00010.
Mekhail N, Costandi S, Nageeb G, Ekladios C, Saied O. The durability of minimally invasive lumbar decompression procedure in patients with symptomatic lumbar spinal stenosis: Long-term follow-up [published online ahead of print, 2021 May 4]. Pain Pract. 2021;10.1111/papr.13020. doi:10.1111/papr.13020
Friedly JL, Comstock BA, Turner JA, et al. Long-Term Effects of Repeated Injections of Local Anesthetic With or Without Corticosteroid for Lumbar Spinal Stenosis: A Randomized Trial. Arch Phys Med Rehabil. 2017;98(8):1499-1507.e2. doi:10.1016/j.apmr.2017.02.029
Pope J, Deer TR, Falowski SM. A retrospective, single-center, quantitative analysis of adverse events in patients undergoing spinal stenosis with neurogenic claudication using a novel percutaneous direct lumbar decompression strategy. J Pain Res. 2021;14:1909-1913. doi: 10.2147/JPR.S304997
Pryzbylkowski P, Bux A, Chandwani K, et al. Minimally invasive direct decompression for lumbar spinal stenosis: impact of multiple prior epidural steroid injections [published online ahead of print, 2021 Aug 4]. Pain Manag. 2021;10.2217/pmt-2021-0056. doi:10.2217/pmt-2021-0056
Abstract presented at: American Society of Pain and Neuroscience Annual Conference; July 22-25, 2021; Miami Beach, FL.
Mobility Matters: Low Back Pain in America, Harris Poll Survey, 2022. View data and full summary here.
Deer TR, Grider JS, Pope JE, et al. Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST): Consensus Guidance from the American Society of Pain and Neuroscience (ASPN). J Pain Res. 2022;15:1325-1354. Published 2022 May 5. doi:10.2147/JPR.S355285.