Identify Neurogenic Claudication Symptoms
- Presents as discomfort in back, legs or buttocks with ambulation that improves with flexion - often referred to as “shopping cart syndrome.”
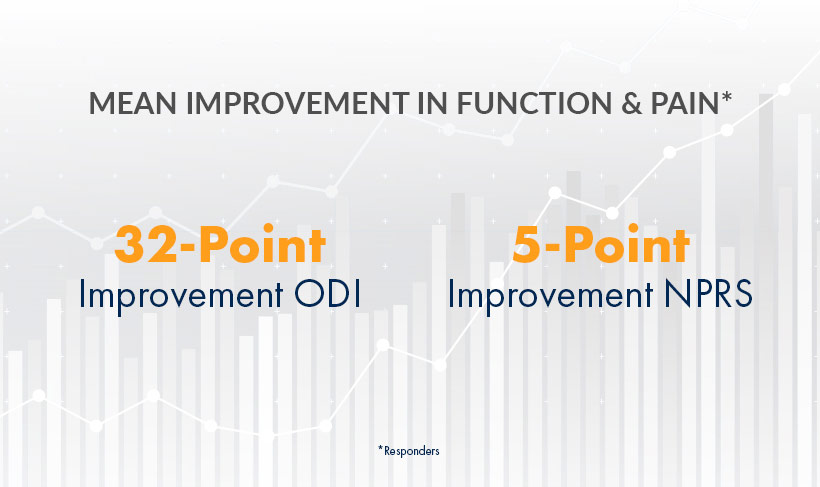
MiDAS ENCORE 2-Year, Level 1 Study: mild® provides clinically meaningful, statistically significant improvements in mobility, ODI, and pain reduction on the NPRS.
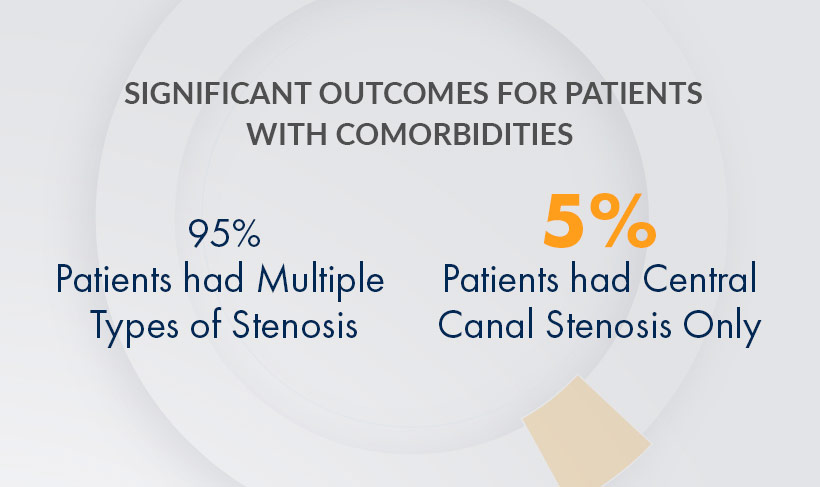
MiDAS ENCORE 2-Year, Level 1 Study: mild® is effective in treating patients with multiple stenosis types, including lateral and foraminal stenosis.

MiDAS ENCORE 2-Year, Level 1 Study: mild® has an equivalent safety profile to an ESI, but with lasting results. In this study, there were no statistically significant differences in the safety profile between study groups.
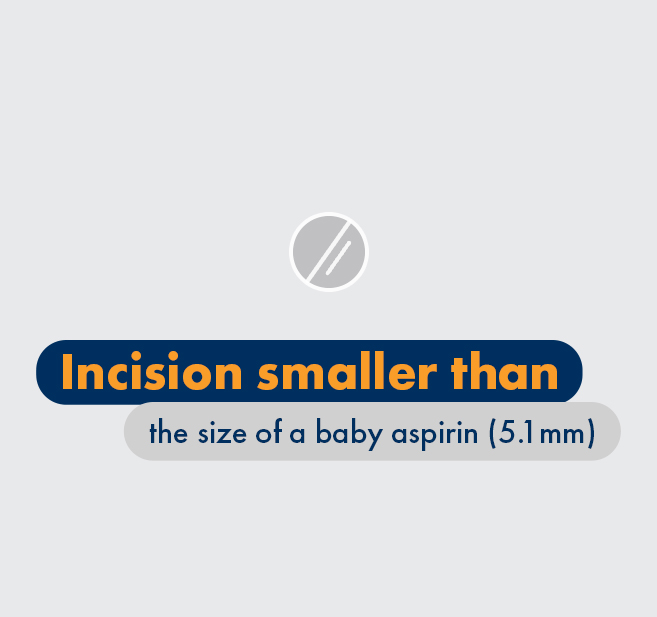
mild® is a minimally invasive procedure typically performed in an outpatient setting using local anesthetics and light sedation. The nature of the procedure carries that do not apply to receiving an epidural steroid injection.

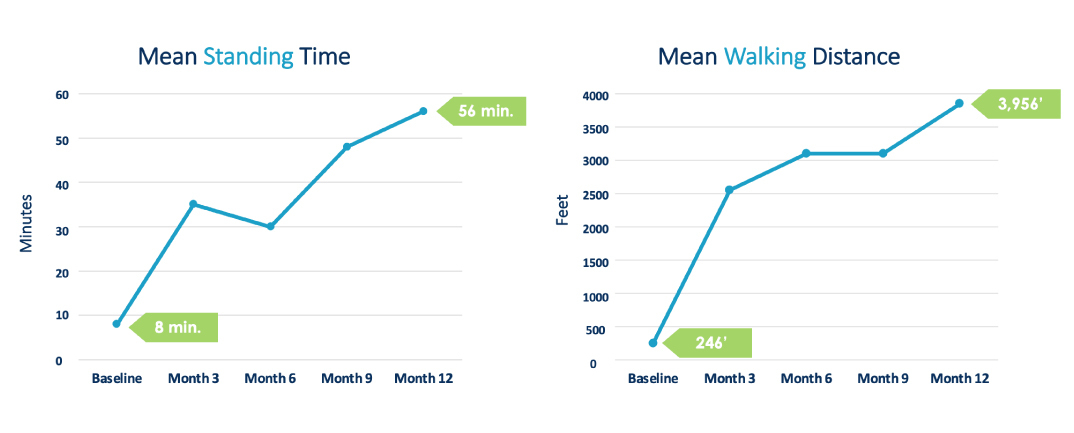
Cleveland Clinic 1-Year Study: Patients’ average standing time improved from 8 min. to 56 min. and average walking distance increased from 246 ft. to 3,956 ft.

Cleveland Clinic 5-Year Study: 88% of mild® patients avoided back surgery for at least 5 years while experiencing significant symptom relief.

MiDAS ENCORE 2-Year Study: Patients reported an 85% patient satisfaction rate with the mild® Procedure.
HLF contributes up to 85% of spinal canal narrowing.
Several cross disciplinary leaders in the interventional spine community, representing many surgical and pain societies, have formed a consensus group to evaluate the current state of LSS diagnosis and treatment, and to make recommendations to guide clinical practice in this emerging area.
With new therapies emerging, you can now think differently about treating LSS patients. Move beyond palliative therapies and address a major root cause of LSS, without leaving any implants behind. If HLF is present, advance to mild® to provide patients long-term relief using a therapy that has a safety profile equivalent to an ESI, but with lasting results.








1

2

3
Familiarity with fluoroscopic imaging techniques and expertise in the epidural space are key qualification requirements for performing mild®.
Publication— Interventional Pain Medicine, 2024
Author— Staats PS, Dorsi MJ, Reece DE, Strand NH, Poree L, Hagedorn JM
Publication— Journal of Pain Research, 2023
Author— Hongjie Yuan, Xiaobin Yi
Publication— PAIN Practice, 2023
Author— Deer TR, Chafin TB, Costandi SJ, et.al.
Publication— Cureus, 2023
Author— Malik KN, Giberson C, Ballard M, et.al.
Publication— PAIN Practice, 2023
Author— Staats P, Hagedorn J, Reece E, et al.
Publication— Journal of Pain Research, 2022
Author— Sayed D, Grider J, Strand N, et al.
Publication— Journal of Pain Research, 2022
Author— Deer TR, Grider JS, Pope JE, et al.
Publication— Pain Medicine, 2022
Author— Deer T, Costandi S, Washabaugh E, et al.
Publication— Pain Management, 2021
Author— Pryzbylkowski P, Bux A, Chandwani K, et al.
Publication— Pain Management, 2021
Author— Pryzbylkowski P, Bux A, Chandwani K, et al.
Publication— Journal of Pain Research, 2021
Author— Pope JE, Deer TR, Falowski SM
Publication— Journal of Pain Research, 2021
Author— Deer T, Kim C, Wahezi SE, Qu H, Sayed D
Publication— PAIN Practice, 2021
Author— Mekhail N, Costandi S, Nageeb G, et al.
Publication— Pain Management, 2020
Author— Jain S, Deer TR, Sayed D, et al.
Publication— Medical Devices (Auckland), 2020
Author— Mekhail NA, Costandi SJ, Armanyous S, et al.
Publication— PAIN Practice, 2019
Author— Deer, TR, Grider JS, Pope JE, et al.
Publication— Pain Physician, 2016
Author— Benyamin RM, Staats PS
Publication— PAIN Practice, 2015
Author— Udeh BL, Costandi S, Dalton JE, Ghosh R, Yousef H, Mekhail N.
Publication— Regional Anesthesia & Pain Medicine, 2018
Author— Staats PS, Chafin TB, Golovac S, et al.
Publication— Pain Physician, 2016
Author— Staats PS, Benyamin RM
Publication— PAIN Practice, 2013
Author— Chen H, Kelling J
Publication— PAIN Practice, 2012
Author— Brown LL
Publication— PAIN Practice, 2012
Author— Mekhail N, Vallejo R, Coleman MH, Benyamin RM
Publication— Pain Physician, 2012
Author— Deer TR, Kim CK, Bowman RG, Ranson MT, Yee BS
Publication— PAIN Practice, 2012
Author— Mekhail N, Costandi S, Abraham B, Samuel SW
Publication— The Clinical Journal of Pain, 2012
Author— Wong WH
Publication— The Clinical Journal of Pain, 2012
Author— Basu S
Publication— Pain Medicine, 2012
Author— Levy RM, Deer TR
Publication— Pain Management, 2012
Author— Deer TR
Publication— Journal of Neurosurgery: Spine, 2011
Author— Chopko BW
Publication— The Neuroradiology Journal, 2011
Author— Schomer DF, Solsberg D, Wong W, Chopko BW.
Publication— Neurosurgical Review, 2011
Author— Deer TR, Mekhail N, Lopez G, Amirdelfan K
Publication— Pain Physician, 2010
Author— Deer TR, Kapural L
Publication— Pain Physician, 2010
Author— Chopko BW, Caraway DL
Publication— Pain Physician, 2010
Author— Lingreen R, Grider JS
Vertos can assist with setting up claims and address any questions you may have. As a general notice, Vertos provides procedure-specific information about codes that may be used for procedures that employ our technology and products. Reimbursement methods vary by payor and site of service.
As commercial insurance coverage for the mild® Procedure varies by payor policy, we encourage providers to contact non-Medicare payors to confirm coverage prior to performing the procedure. If you have questions or are interested in commercial policy advocacy, please contact our Market Access Team.
(855) 848-6453
Learn more about the mild® Procedure through didactic lectures, discussions and a compendium of case reviews from other leading experts.
Access On-Demand WebcastsPlease see the Vertos Medical guide for simple claim set-up instructions and contact information.
Download Billing GuideThe Vertos mild® Devices are a sterile, single-use system of specialized lumbar decompression surgical tools used to remove small portions of the lamina and preferentially resect and debulk the thickened ligamentum flavum.
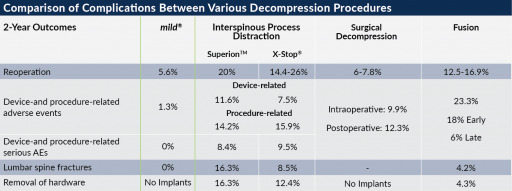
Download IFUClick here to view the “Minimally Invasive Lumbar Decompression: A Review of Indications, Techniques, Efficacy and Safety” and references for this chart.
All lumbar levels, including L5-S1, are treatable with mild®. The physician should decide which levels to treat based on symptom and imaging assessment.
Patients typically resume normal activity within 24 hours with no restrictions after having the mild® Procedure. Many patients notice an improvement in their ability to stand longer and walk farther within a few days, as shown in the Functional Outcome Improvement charts from the Cleveland Clinic Study at 1-Year below, and in some cases immediately after having mild®.
For some patients, it’s a matter of rebuilding strength after being deconditioned by the debilitating effects of LSS, such as a limited ability to walk. In these cases, it may take three to twelve months post-mild® to achieve full benefits.
Yes. mild® doesn’t cause major anatomical changes and therefore doesn’t burn bridges if other treatments are required in the future. mild® does not eliminate any treatment options.
The physician would need to assess the patient’s health and disease state to identify if the patient is a candidate. Typically, if the physician can access the HLF safely, mild® can be performed.
mild® is currently reimbursed in the outpatient hospital or ASC setting.
Yes, the mild® Procedure is covered nationwide by Medicare and Medicare Advantage. Commercial coverage and other plans vary. View our .
In collaboration with the nation’s leading mild® practitioners, we provide training and education to physicians and practices across the US. Visit the Training & Education section above to learn more.
Please complete the contact form and someone will get back to you shortly.
Vertos Medical provides a variety of print and digital resources to mild® providers to help educate their patients and staff. Please contact your local representative or contact us for assistance.
Our long-term vision is to create global patient access to the mild® therapy. We are actively planning for international expansion and have a CE Mark, but are not yet ready to initiate our efforts. To stay updated on our progress, please visit our website’s newsroom.
To better serve the healthcare community, a CED study was conducted to obtain national Medicare coverage for the mild® Procedure. During the time that we focused on those efforts, active selling was temporarily paused until the current national Medicare coverage policy was issued. There were no product defects, safety issues or regulatory concerns associated with the pause.

Celebrating over 100,000 mild® PATIENTS at ASPN 2024!
Dr. David Dickerson and other leading mild® providers captivated a packed room with their insights on how they elevated their practice with mild®. Attendees learned the latest clinical findings and proven strategies to expand patient access and build a thriving practice with mild®. mild® providers were also able to share success stories recorded live at our custom recording booth!
This study measures the impact of the mild® Procedure as a first-line therapy on patients otherwise receiving conventional medical management (CMM) for lumbar spinal stenosis (LSS) with neurogenic claudication (NC) secondary to hypertrophic ligamentum flavum. It demonstrated that the mild® Procedure, when combined with CMM, is superior in providing improved function and decreased pain when compared to CMM alone. These results provide support for early interventional treatment of symptomatic LSS with the mild® Procedure.
Benyamin RM, Staats PS, MiDAS ENCORE Investigators. mild® is an effective treatment for lumbar spinal stenosis with neurogenic claudication: MiDAS ENCORE Randomized Controlled Trial. Pain Physician. 2016;19(4):229-242.
Mekhail N, Costandi S, Abraham B, Samuel SW. Functional and patient-reported outcomes in symptomatic lumbar spinal stenosis following percutaneous decompression. Pain Pract. 2012;12(6):417-425. doi:10.1111/j.1533-2500.2012.00565.x.
2012 data from Health Market Sciences report for Vertos Medical 2013.
Data on file with Vertos Medical.
Staats PS, Chafin TB, Golvac S, et al. Long-term safety and efficacy of minimally invasive lumbar decompression procedure for the treatment of lumbar spinal stenosis with neurogenic claudication: 2-year results of MiDAS ENCORE. Reg Anesth Pain Med. 2018;43:789-794. doi:10.1097/AAP.0000000000000868.
Based on mild® Procedure data collected in all clinical studies. Major complications are defined as dural tear and blood loss requiring transfusion.
MiDAS ENCORE responder data. On file with Vertos Medical.
Jain S, Deer TR, Sayed D, et al. Minimally invasive lumbar decompression: a review of indications, techniques, efficacy and safety. Pain Manag. 2020;10(5). https://doi.org/10.2217/pmt-2020-0037. Accessed June 1, 2020.
Deer TR, Grider JS, Pope JE, et al. The MIST Guidelines: the Lumbar Spinal Stenosis Consensus Group guidelines for minimally invasive spine treatment. Pain Pract. 2019;19(3)250-274. doi:10.1111/papr.12744.
Hansson T, Suzuki N, Hebelka H, Gaulitz A. The narrowing of the lumbar spinal canal during loaded MRI: the effects of the disc and ligamentum flavum. Eur Spine J. 2009;18(5):679-686. doi:10.1007/s00586-009-0919-7.
Treatment options shown are commonly offered once conservative therapies (e.g., physical therapy, pain medications, chiropractic) are not providing adequate relief. This is not intended to be a complete list of all treatments available. Doctors typically recommend treatments based on their safety profile, typically prioritizing low risk/less aggressive procedures before higher risk/more aggressive procedures, but will determine which treatments are appropriate for their patients.
The mild® Procedure is a minimally invasive treatment for lumbar spinal stenosis. As with most surgical procedures, serious adverse events, some of which can be fatal, can occur, including heart attack, cardiac arrest (heart stops beating), stroke, and embolism (blood or fat that migrates to the lungs or heart). Other risks include infection and bleeding, spinal cord and nerve injury that can, in rare instances, cause paralysis. This procedure is not for everyone. Physicians should discuss potential risks with patients. For complete information regarding indications for use, warnings, precautions, and methods of use, please reference the devices’ Instructions for Use.
Patient stories on this website reflect the results experienced by individuals who have undergone the mild® Procedure. Patients are not compensated for their testimonial. The mild® Procedure is intended to treat lumbar spinal stenosis (LSS) caused by ligamentum flavum hypertrophy. Although patients may experience relief from the procedure, individual results may vary. Individuals may have symptoms persist or evolve or other conditions that require ongoing medication or additional treatments. Please consult with your doctor to determine if this procedure is right for you.
Reimbursement, especially coding, is dynamic and changes every year. Laws and regulations involving reimbursement are also complex and change frequently. Providers are responsible for determining medical necessity and reporting the codes that accurately describe the work that is done and the products and procedures that are furnished to patients. For this reason, Vertos Medical strongly recommends that you consult with your payers, your specialty society, or the AMA CPT regarding coding, coverage and payment.
Vertos Medical cannot guarantee coding, coverage, or payment for products or procedures. View our Billing Guide.
Vertos is an equal employment opportunity workplace committed to pursuing and hiring a diverse workforce. We strive to grow our team with highly skilled people who share our culture and values. All qualified applicants will receive consideration for employment without regard to sex, age, color, race, religion, marital status, national origin, ancestry, sexual orientation, gender identity, physical & mental disability, medical condition, genetic information, veteran status, or any other basis protected by federal, state or local law.
Hall S, Bartleson JD, Onofrio BM, Baker HL Jr, Okazaki H, O’Duffy JD. Lumbar spinal stenosis. Clinical features, diagnostic procedures, and results of surgical treatment in 68 patients. Ann Intern Med. 1985;103(2):271-275. doi:10.7326/0003-4819-103-2-271.
Kalichman L, Cole R, Kim DH, et al. Spinal stenosis prevalence & association with symptoms: The Framingham Study. Spine J. 2009;9(7):545-550. doi:10.1016/j.spinee.2009.03.005.
Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998;14(2):148-151. doi:10.1097/00002508-199806000-00010.
Mekhail N, Costandi S, Nageeb G, Ekladios C, Saied O. The durability of minimally invasive lumbar decompression procedure in patients with symptomatic lumbar spinal stenosis: Long-term follow-up [published online ahead of print, 2021 May 4]. Pain Pract. 2021;10.1111/papr.13020. doi:10.1111/papr.13020
Friedly JL, Comstock BA, Turner JA, et al. Long-Term Effects of Repeated Injections of Local Anesthetic With or Without Corticosteroid for Lumbar Spinal Stenosis: A Randomized Trial. Arch Phys Med Rehabil. 2017;98(8):1499-1507.e2. doi:10.1016/j.apmr.2017.02.029
Pope J, Deer TR, Falowski SM. A retrospective, single-center, quantitative analysis of adverse events in patients undergoing spinal stenosis with neurogenic claudication using a novel percutaneous direct lumbar decompression strategy. J Pain Res. 2021;14:1909-1913. doi: 10.2147/JPR.S304997
Pryzbylkowski P, Bux A, Chandwani K, et al. Minimally invasive direct decompression for lumbar spinal stenosis: impact of multiple prior epidural steroid injections [published online ahead of print, 2021 Aug 4]. Pain Manag. 2021;10.2217/pmt-2021-0056. doi:10.2217/pmt-2021-0056
Abstract presented at: American Society of Pain and Neuroscience Annual Conference; July 22-25, 2021; Miami Beach, FL.
Mobility Matters: Low Back Pain in America, Harris Poll Survey, 2022. View data and full summary here.
Deer TR, Grider JS, Pope JE, et al. Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST): Consensus Guidance from the American Society of Pain and Neuroscience (ASPN). J Pain Res. 2022;15:1325-1354. Published 2022 May 5. doi:10.2147/JPR.S355285.