Know Your Back Story: A National Health Awareness Campaign
Published January 25, 2023
Could Knowing Your “Back Story” Help You Rewrite Your Future?
Vertos Medical is proud to have joined forces with the American Society of Pain & Neuroscience (ASPN) and the National Association of Memoir Writers (NAMW) to develop the Know Your Back Story campaign, a national public health awareness campaign that seeks to help patients suffering from chronic low back pain (CLBP) learn more about their “back stories.” The campaign encourages providers to educate their patients on lumbar spinal stenosis (LSS) and provide awareness around the enlarged ligament that may be causing their pain.
Vertos Medical is committed to empowering healthcare providers and patients with minimally invasive treatments for LSS, and the Know Your Back Story campaign plays a significant role in fulfilling our core mission: to help patients suffering from chronic back pain reclaim their quality of life using the simplest, safest, most durable, and earliest treatment available.
The Prevalence of Chronic Low Back Pain
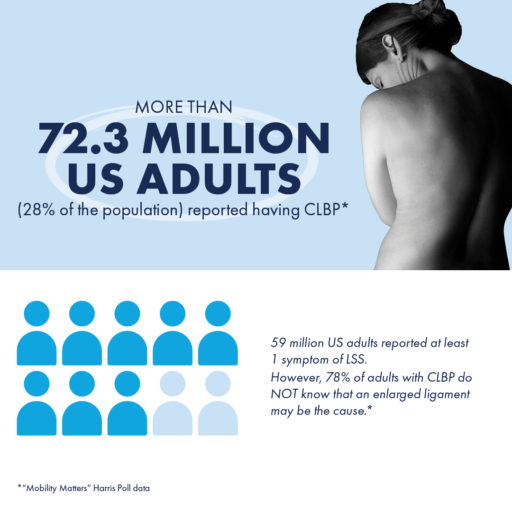
As part of the Know Your Back Story campaign, we partnered with The Harris Poll to conduct a landmark survey on CLBP in the United States. Results from the “Mobility Matters: Chronic Low Back Pain in America” survey indicate that CLBP affects more people than arthritis, diabetes, or heart disease, but over one-third of CLBP patients have never been told by a provider what the exact cause of their pain is.
The Need for Increased Patient Education
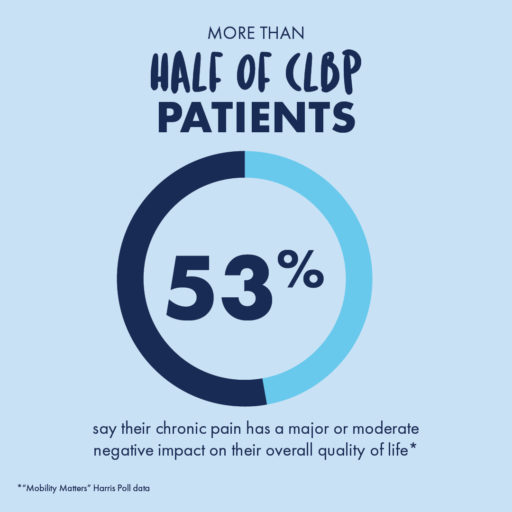
“Mobility Matters: Landmark Survey on Chronic Low Back Pain in America” also revealed misconceptions about CLBP and the need for education about the associated impacts on mobility and quality of life, and where to go to for diagnoses and information about available treatment options.
Finding the Right Doctor
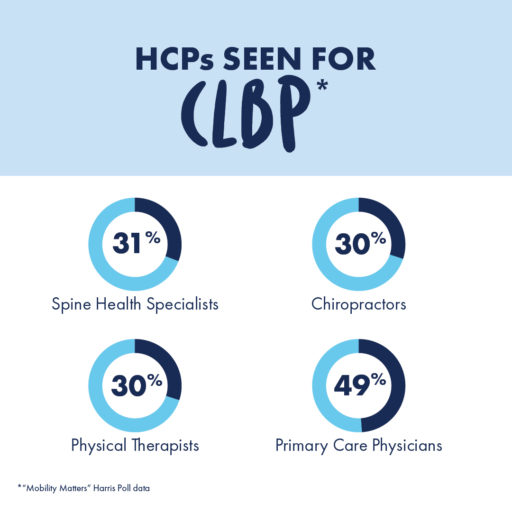
The average chronic low back pain sufferer has seen at least 3 different healthcare professionals (HCPs) seeking treatment for their pain and has made 4 visits to an HCP within the last year.
For the most accurate diagnoses and treatment recommendations that may lead to lasting relief, patients should seek out doctors who specialize in spine health, such as pain specialists, physical medicine, and rehabilitation (PM&R) physicians, interventional pain physicians, or physiatrists.
By meeting with doctors who specialize in spine health, patients may be able to gain new insights into the root cause of their pain.
LSS: The Often-Overlooked Cause of CLBP
Lumbar spinal stenosis (LSS) is a condition, prevalent in approximately 20% of patients over the age of 60, in which the lower spinal canal narrows and compresses the nerves in the lower back. Up to 85% of spinal canal narrowing is caused by an enlarged ligament.
This pressure around the spinal cord can cause pain, numbness, heaviness, or tingling in the low back, legs, and buttocks, but the vast majority of CLBP patients have never heard of this potential diagnosis.
The Know Your Back Story campaign’s objective is to spread awareness around LSS and get more patients on the path to lasting relief. By collecting intensive data, developing tools for patient education, and sharing insights with both patients and providers about the effects of LSS and its potential treatment options, the Know Your Back Story campaign has served as a significant step in bringing more visibility to this condition.
Get To Know Your Back Story
Getting screened for LSS and CLBP can open the door to learning more about treatment options available, such as the mild® Procedure.
Introducing the First-Of-Its-Kind Mobility Index
One of the key accomplishments of the Know Your Back Story campaign is the development of the first-ever Mobility Index, a breakthrough resource for demonstrating the differences in mobility and quality of life between patients with CLBP and their peers without CLBP.
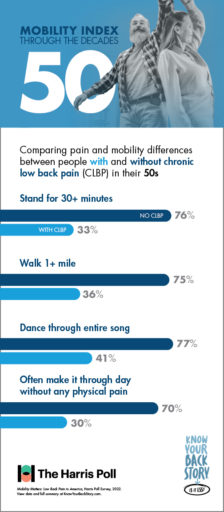
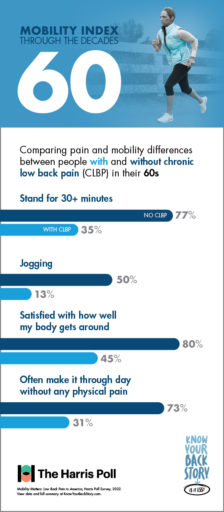
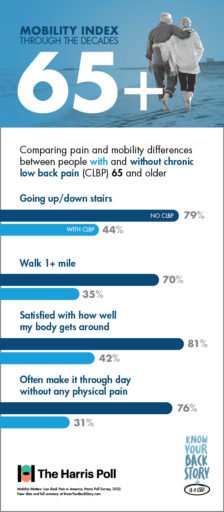
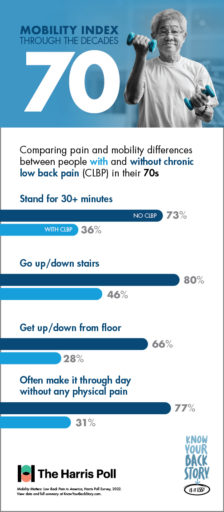
Results from the “Mobility Matters: Landmark Survey on Chronic Low Back Pain in America” conducted by The Harris Poll show that with age, CLBP patients experience significantly greater challenges performing physical tasks and making it through the day without pain or limited mobility than others within their age group without low back pain.
For instance, nearly 3 in 4 individuals in their 50s who do not suffer from CLBP are able to easily stand for half an hour or longer. In contrast, the number of CLBP patients in the same age range who are able to do the same is just over 3 in 10.
When it comes to other activities such as walking, dancing, or using the stairs, the Mobility Index can be a great tool for educating patients. By reviewing the differences in mobility between similar individuals with and without CLBP, patients can understand more about what chronic pain is keeping them from—and their options for finding lasting relief.
Bringing the Know Your Back Story Campaign to the Public
On the quest to educate, engage, and increase awareness within communities, the Know Your Back Story campaign took the #LookForTheLigament Education and Experiential Mobile Unit on tour down the East Coast, stopping in New York City, NY; Philadelphia, PA; Washington, D.C.; and Sarasota, West Palm Beach, and Miami, FL.
The mission of this tour was to encourage people suffering from CLBP to get screened for LSS and an enlarged ligament by a spine health doctor, and to provide both patients and HCPs with an in-depth look at the causes and effects of LSS through interactive experiences and demonstrations, including:
- Visualization stations that explored why LSS symptoms occur, tips on how to identify symptoms, how an enlarged ligament impacts spine health, and the potential for the mild® Procedure as a treatment option.
- An immersive 3D journey down the spinal canal to the lumbar region that explored the enlarged ligament, spine degeneration, and how mild® works.
- The Interactive Ligament Kiosk, which featured Mobility and the Enlarged Ligament, an animated educational program that demonstrated the inherent spinal compression associated with the diagnosis of LSS and its effect on pain, posture, and mobility; a Look for the Ligament interactive opportunity for people to view and compare MRI images of how a healthy ligament should look against imaging of an enlarged ligament; and a How Do Doctors Describe LSS? module filled with a colorful list of analogies and explanations doctors often use to describe the condition to their patients.
- Interactive Motion Memoir iPads, featuring our writing program developed with award-winning author, certified therapist, and founder of the National Association of Memoir Writers (NAMW), Dr. Linda Joy Meyers, who provided tips and encouragement to help patients trace their own history of low back and leg pain to visualize the next chapter of their potentially pain-free life.
Watch the Video to See More Highlights From the #LookForTheLigament Tour:
Getting Involved as a Healthcare Provider
By staying aware of the impacts of LSS and CLBP on patients’ mobility and potential treatment options, healthcare providers can help more patients in their communities get on the path to lasting relief. By working alongside others in their practice or by creating referral networks with primary care, physical therapy providers, and other local providers, HCPs in Interventional Pain Management (IPM) or spine health specialties can play a more effective role in identifying patients suffering with LSS or CLBP and connect them to providers that are able to offer more durable treatment options.
Physicians and Advanced Practice Providers (APPs) can also play a more proactive role in identifying LSS by staying aware of common patient misconceptions about back pain. By utilizing the tools and resources developed as part of the Know Your Back Story campaign, you can keep your patients as educated as possible about the potential causes of their chronic pain, as well as the treatment options that may finally provide them with relief.
Hear From Patients
How Patients Can Find Relief
For patients looking to learn more about the source of their pain and their options for relief, finding a local spine health doctor is a crucial first step. By using the MD Finder tool, patients can find doctors in their area who may be able to provide the answers they’ve been seeking.
A spine health specialist can help walk patients through their options for treatment, from more conservative therapies such as medication or physical therapy to longer lasting, minimally invasive treatments such as the mild® Procedure.
How mild® Makes a Difference
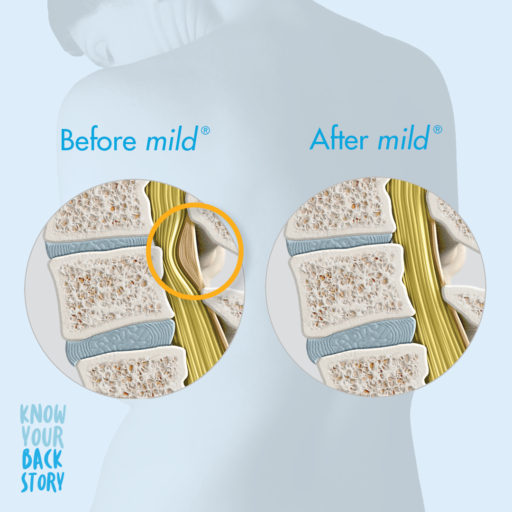
The mild® Procedure, or minimally invasive lumbar decompression, may be pursued as a first-line therapy for LSS.
A minimally invasive procedure that is considered the gold standard of care in LSS treatment, mild® addresses a major root cause of LSS by debulking the enlarged ligament to restore space in the spinal canal and reduce compression of the nerves. With a safety profile equivalent to an epidural steroid injection (ESI), mild® has helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief,—a durable, lower-risk treatment option to spacer implants or open surgery.

For patients considering mild®, the Move More Questionnaire is a great resource for identifying current limitations and tracking their reduced pain and improved mobility after the procedure.
By becoming familiar with the Know Your Back Story campaign and exploring the insights and resources developed to spread awareness about LSS, both patients and providers can help spread the word about this under-diagnosed cause of CLBP.
Vertos Medical is committed to helping patients experiencing chronic pain reclaim their quality of life with a short, minimally invasive early treatment option with the mild® Procedure, both through the Know Your Back Story campaign and in everything we do.