02:40
Kris Krustangel
Yeah, thanks for having me. I feel really lucky to be a part of this conversation today.
02:44
Podcast Host
So you’ve been in med device a long time, a lot of different roles, a lot of different responsibilities. And kind of, to my statement earlier, I know some conversations we’ve had before that you’ve realized at times that ego could be an obstacle and were talking about The Obstacle is the Way and things of that nature, along with stoic philosophy. Was there a moment in time throughout your career that you sort of had that revelation? Did you just walk out of an opportunity or what was that?
03:14
Kris Krustangel
Yeah, just give a little context: so it’s been 20 years of medical device. I started as a clinical specialist and kind of grown from that role into now leadership for the last 12 or 13 years. But to answer your question specifically, it was about like year into my first leadership role where I can just remember, you know, coming out of a QBR (quarterly business review) and being so focused on really, you know, how I looked, how the slides looked, how my answer sounded. I was kind of void of really the authenticity of driving the real solution to the problem. And I remember coming out of the meeting, and I’m sure you guys have been in these meetings, right? You got like 20 managers and a couple of VPs, and they’re grilling you and you come out…
03:51
Kris Krustangel
At that moment, my pride was pretty high, and I had kind of an adjacent leader who wasn’t my VP, who was a VP in there. He’s like, “you kind of crapped the bed in there.”
04:00
Kris Krustangel
What? What do you mean I crapped the bed? He’s like, I’m not really sure you answered many of the questions that were being asked. I mean, yeah, it looked good and it sounded good, but I’m not sure it really delivered in the way. And man, I still to this moment, remember that individual and thank him all the time when I see him at conference because it was kind of a seminal moment when I realized like what were my priorities as a leader specifically? Like what was I trying to show up and do and most importantly, how to be effective. So, yeah, that one to this day, I remember were like in Huntington Beach. I remember the room. I remember he grabbed me on that thing, you know, the awning right outside. And I was just too focused on looking good, I’ll be honest.
04:34
Kris Krustangel
And it was a mistake at a time in my career. I’m really grateful that happened early in my leadership career, for sure.
04:38
Podcast Host
That’s awesome, man. I love to hear that someone cared enough to pull you aside because that means they didn’t care how they looked, right?
04:49
Kris Krustangel
Yeah. Isn’t that true? That’s true. So, so true.
04:52
Podcast Host
That’s awesome. So you experienced that and you remember the room, probably the smell, everything about that day. What did you do about it?
05:01
Kris Krustangel
That’s a great question, and I think it’s iterative. Like, I didn’t wake up the next day and become my best version of myself. You know how it is. Just like you said in the beginning of this podcast, it’s about growing yourself and growing thoughts. So it takes time. But I think I was able to firstly kind of refocus on what matters most. And a lot of times, it’s not what matters to you. It’s what matters to those that are around you, right? So being kind of selfless first. And so you take the example of the questions that I was tasked with answering. I wasn’t really paying attention to the core of those questions, which are just like some business foundational things.
05:34
Kris Krustangel
And so I went back and I dug back in with my team and really tried to come up with better answers that were focused, that maybe didn’t look good. Right. Maybe weren’t doing the things were supposed to be doing, but they got up before the answer. And then I actually went back and took it back and had a sidebar with my VP at the time to kind of fill in those answers. And it felt, I don’t know, kind of invigorating because after that conversation, you know, sometimes the world gives you feedback right away. There’s real tactical, practical feedback with also resources to actually solve the problems versus me just, again, looking good. So it was iterative. Like I said, I came back, I tried to internalize it.
06:06
Kris Krustangel
I talked to my team, and then I tried to present something just as that kind of like, first step to “am I back on the right path or am I back on the correct path?” And I got some pretty quick feedback to say, yeah, this is the way at least you should think about leading in the medical device world. And it’s been pretty consistent since that.
06:22
Podcast Host
Yeah, I’m curious. This might be a strange question, but if you look back on the idea of wanting to look good, do you have a sense of what that was a symptom of that led you to that point at that time?
06:38
Kris Krustangel
That’s a deep question. You know, one, I’m not a good-looking guy here watching this on the camera. [Laughs] So it’s not that, you know, I think it comes down to earlier in careers and maybe earlier in tenures of positions. We’re all kind of feeling our purpose and our way out, and with the ways that we’re seeing, if that makes sense. And sometimes I think it’s easy to overcompensate with movements and actions and even volume, like just how loud you are versus substance. And I don’t think it’s anybody’s fault. I mean, for those of the people that are listening, that are in medical device, we see it every day. I see it with doctors, I see it with reps, I see it with other leaders.
07:14
Kris Krustangel
But I tend to realize that it’s those people that can have either someone stop them to point out the gap or someone to really self-actualize as life just goes on, you’re more comfortable. That’s not the most important thing to think about. But to answer your question again, it feels circumstantial. You know what I mean? Like, it’s just a way. Sometimes you start in a position, and I think it’s totally normal. I bet you people on the call right now feel the same way, and it’s totally normal. Not that you’re asking me this, but I think the challenge is like, how quickly can you realize that’s not the most important thing? And then how can you elevate yourself to put yourself in a position where you’re really delivering value, whatever you’re doing, right?
07:50
Podcast Host
Yeah, it’s pretty fascinating because I could almost see it turning into like a Pavlov’s dog scenario. Like we experience the success around something and so we associate these things, but maybe it’s correlation, not causation, but then our brain goes, well, I gotta be this way. So, yeah, it’s great for you to identify how has it changed how you look at business today. Does it impact your conversations with the team hiring? How does that look?
08:20
Kris Krustangel
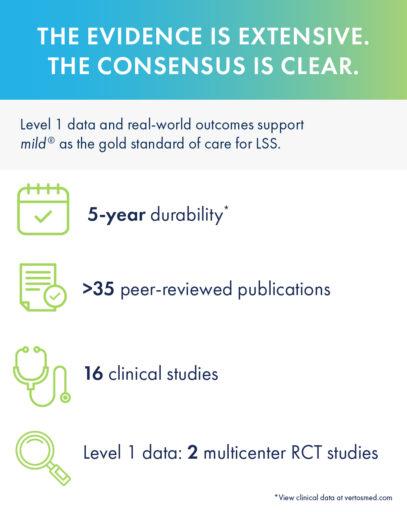
It 100% does. And I won’t go too far back into my story, but, you know, I’ve had a series of different experiences with large strategics as well as, you know, very small startups, being commercial employee number one. Now, Vertos Medical, where I call it a middle-sized startup, but, you know, as I went through my due diligence before I had the opportunity to really join here. I mean, I looked through a pretty critical lens about how decisions are made, right? What the mission of the organization is and how ultimately the resources align up with those things. And I think what you learn if you start to get a real eye for ego, is that that ends up being an obstacle. To your point at the beginning, that ego is the enemy.
08:58
Kris Krustangel
And so when you see those things, I think you’re able to either do one of two things. You can make a decision about just not engaging, right? Like, I’m not gonna go down this path. Like, and again, for people listening, with all due respect, I’m sure there’s a physician, you know, that has a certain bravado or whatever, and you just realize the amount of resource and time you’re gonna have to spend to convert or get to that position. You have to ask, is it worth it? So there’s an engagement decision to make. And then the second part is, once you’ve made that decision to engage, how are you going to adapt in a way that’s still meaningful to move forward, whatever that mission or that purpose is.
09:30
Kris Krustangel
And I think in everything that I do, I’m looking for it to a fault or to a betterment because it allows me to be more functional, more fluid. Now, what I just pointed out where situations where I’m relying on, like a physician, right, or a sale. Only as my team, it makes it a little bit easier because I can just point it out, you know what I mean? Like, granted, I do it in a very compassionate way. I mean, my mantra is challenge directly, care compassionately. So I’m definitely direct. But I’m also, I would like to say, do it have a kind heart because I care about the people I’m connected with. But in the team that I work on, obviously the rules are a little bit different.
10:02
Kris Krustangel
I can just basically go to you and say, like, is this the best decision for the business? Or do you like this decision because you came up with it and be honest about it too? Like, and I’ve been there, too. We all have. And I think being able to see that environment in business play out in real time, there’s no question in my mind the better that we get at that last version of what I just explained to you, we come up with faster, better solutions to deliver value to our patients and physicians—with no doubt in my mind. So not only do I look at it, not only am I conscious of do I engage with it? But professionally, now I’m trying to drive it.
10:34
Kris Krustangel
I’m trying to drive an environment where we remove ego and really focus on the best decisions for the business to help the patients and physicians we work with. So great question.
08:02
Podcast Host
Have you noticed this mindset? I guess first, let me ask this. Let’s say someone is listening and they’re interested in this concept, this idea. It maybe rings familiar to them, but maybe they never put words to it or a structure. You mentioned Ryan Holiday. Are there any other sources of content that you have found yourself going to learn more about the actual operating system of what this looks like from a behavioral standpoint?
11:11
Kris Krustangel
I could give you a bunch of recommendations, but truthfully, if you’re looking to start with Ryan Holiday, he has a book called Ego is the Enemy. There’s another one called The Obstacle is the Way. They’re very closely aligned. It’s based on stoic philosophy, which sounds way smarter than a state school-graduated guy like me. But the foundational principles are all there. And if you start with either of those books, or even just the blogs or the podcasts he does, it’ll give you a taste of what he’s talking about. And a lot of it is what I like to think is just air that we breathe already. You know what I mean? Be kind, be honest. Like, these aren’t new concepts. But I think the way he talks about it, and he gives experiences or descriptions of how it fits in everyday life…
11:48
Kris Krustangel
Like, he does it for being a father, he does it for being a friend, he does it for being a professional. You actually start to see the architecture, right? The beams of the building in front of you in different places, and that’s really helpful. And then he does go on and there’s other kind of step offs from him to talk about how it applies to business. So I’d definitely just start there. It’s too good to go anywhere else, honestly. He’s kind of the mecca on this topic, on modern day stoicism, for sure.
12:12
Podcast Host
Yeah. He’s got a lot of study behind it. He frames stoic philosophies in a lot of modern terminology or ways that we communicate today. I’ve read The Obstacle is the Way. I have not read Ego is the Enemy. I definitely need to. He’s also a great writer.
12:27
Kris Krustangel
Totally. Yeah.
12:30
Podcast Host
So I’m curious. You had that shift, and you named it as a seminal shift. You started to pay attention. It was iterative. So over time, you’re recognizing more and more how these changes in your behavior are not only better for the business, but I’m assuming better on the communication with your team, the relationships you built. Did you get any feedback over that course of iteration from direct reports, people that were adjacent to you? Any of those team members?
12:56
Kris Krustangel
Yeah, that’s a great question. I definitely did. I mean, to be really honest with you, I think authenticity is hard. You know what I mean? It feels hard to. Especially. You have almost like, there’s so much noise right now, in the environment, it’s hard to even know when to be authentic versus when you’re being buzzed at by social media or, you know, your phone’s ringing or your dog. Like, when are these moments to be really clear and present? I would say. And wherever you’re doing. And so, to answer your question, it’s like there’s certain situations, whether it be leaders or reps, where at the end of the day, they’re pausing and they’re kind of re-churning all that we talked about—a lot of authentic, challenging, right? A lot of, “Hey, is this the best decision? Is this the right customer?”
13:33
Kris Krustangel
“Have you thought about it?” And again, a kind of compassionate way. And at the end of the day, I do tend to get pretty good feedback. Like, this is a super powerful day. I’m really glad you said this. Nobody’s framed it that way. And I don’t think the way that I say it is special, but I will say that I am overtly focused on being authentic and being really kind about it in a way that matches what they’re trying to do, right? And what matters to them—not just what matters to me, what matters to them. And so I think I tend to get a lot of feedback over time where it’s, you know, the different VPs that I work with now or my CCO or, you know, the reps, like, they appreciate it.
14:08
Kris Krustangel
I think at times I’d be lying if I don’t wear people down a little bit. I mean, they don’t want to hear it, and maybe I don’t want to hear it. I’ll be honest with you. But I just feel deeply passionate and purpose driven around the idea that I can help people do better at what they want to do when I’m not around them especially, that’s the best possible thing I could ever do. For what? In my life, yeah. As a parent, as a professional, like, there’s nothing more important to me than doing that thing. So I’m going to value the time that I have to have those conversations. And generally, yeah, I mean, I get some feedback in the discussion that, like, it’s positive. I’m starting to get—I’ll be very clear—the reps ride with me…
14:47
Kris Krustangel
Like, they don’t want to hear me, but it’s not for everybody, and it’s the price you pay for the space you occupy. But the feedback has been good, and that’s why I continue to kind of double and triple down on being really authentic and direct with my approach and things.
15:00
Podcast Host
What framework are you walking through when you’re not in a good headspace? Or things seem to be crashing around. Right. Which happens frequently for everybody. What framework do you walk through mentally to say, hey, am I staying authentic? Am I being authentic? Like, what does that define that? And then what framework do you use to kind of check yourself? I think that’d be helpful for everybody that’s also looking to do the same thing.
15:22
Kris Krustangel
It’s hard because, you know, I don’t know how I’m coming across right now. People usually say high energy, passionate. I’m not always like this. I have bad days, like, I have bad minutes. I think, to answer your question, it’s okay. First off, just be okay with that. Like, some people feel guilty or they try to avoid it, but, like, just be okay that you’re not your best self. I think that’s the first step of that kind of recovery mindset of what you’re describing. But the second thing is, I do try to spend a little bit of time, whether it be journaling or just discussing with an adjacent peer or mentor, like, what’s really getting at me. Like, I’ll throw out all the practical pieces and say, hey, this is what I think about this thing. What do you think about?
15:55
Podcast Host
And generally, you know, nine times out of ten, eight times out of ten. And again, PSA public service announcement: surround yourself with good people that you can trust, that are better than you, that are going to say stuff to you that you don’t want to always hear because it works. But I have those conversations eight times out of ten, nine times out of ten that give me that perspective of why I’m maybe not feeling authentic or I’m not feeling as connected with the things that I do. And then I try to get back on track. And even to be more practical than that, sometimes it’s just a mood, you know what I mean? You just don’t wake up and you don’t have the best sleep.
13:47
Kris Krustangel
Or I’ve got a teenage son who, you know, wants to talk to me until 02:00 in the morning, which, you know, I really appreciate. Because he’s gonna graduate eventually. But it makes it hard the next day. Maybe I’m not my best self. So I also try to think about things that give me quick boost, which, you know, one of my mentors, Alan Meacham, he’s the chief revenue officer for Nalo Medical. You know, practice gratitude. Just take a quick stock of what you’re thankful for in a moment. Music. Work it out. Even a quick ten-minute set of something like, and maybe that’s a little shallower than you’re looking for, but those are just quick blips to get you kind of back to where you need. And we all need them. I mean, we just, we all need them.
14:22
Kris Krustangel
I think the trick is recognizing how far you’ve gone before you actually realize: oh, I need that thing. And that’s why I go back to the first piece is like, pick up the phone. Hopefully you can talk to somebody that can kind of give you perspective that’s outside of your head.
14:34
Podcast Host
Yeah, I mean, look, we all know this, generally speaking, the med device community is a pretty active, very competitive, pretty fit (generally speaking) community. But this isn’t going to be a shock to anybody. Moving your body, getting a sweat and doing something hard, even if it is for ten minutes—the physical will affect the mental, right? And help clear the headspace. And so you ask, hey, maybe this is a little more, or you made the statement, maybe this is more shallow. Not at all. Those things have real physiological differences when we do them specifically, routinely. And that’s why I was asking. I was curious, what do you do, man? Because anybody in a leadership role, you’re catching the—somebody told me this once, right? one of my own mentors—you never come to me with the good things.
15:17
Podcast Host
You only come to me with the problems. They’re catching everybody’s problems. And so you’ve got to be able to wear that. And still, to your point or to what you’re talking about, remain authentically optimistic, positive, all of those things. So that’s why I was curious, how do you juggle it? Because everybody’s always looking for those little pearls so that they can let the water roll off their back like a duck, right?
15:41
Kris Krustangel
Yeah, totally. Well said. And again, it’s an iterative process. You know, as I learn new things or new tricks and tips, I’m always trying to put it in. But I think what you’re asking around mindset as well as energy management, because I think that’s a part of it, it’s really important. I think it’s under clubbed golf analogy, right. Kind of under invested in medical device. Could we just like go, go? Which don’t get me wrong, I’m guessing the three of us and the vast majority of your listeners, because they’re listening to this, are constantly going and going. But when you’re on that airplane, and they tell you put on the air mask before assisting others—I always believe that there’s something to be said about that.
16:17
Kris Krustangel
If you’re going to function at the highest level possible, if you’re going to show up for others like you do, you really have to show some boundaries to invest in yourself, to provide that energy and mindset so you can stay at that level all the time. And that’s, again, I’m just some medical device leader. I mean, you talk to, like, the Kobe’s and, like, the real performers, they’re the same way, right? They know down to the fraction of the second how to invest their time to recover.
16:39
Podcast Host
Right?
16:39
Kris Krustangel
And that’s what we’re talking about. And so I can’t go by this part of the conversation without throwing out another PSA. Invest in yourself, invest in your energy, invest in your mindset so you can do the hard work when you need to, do the hard work and move whatever you’re trying to do, move forward. So, great fallout.
16:54
Podcast Host
I appreciate that, because the same potential level of ego that could tell us that we need to be able to sleep less, we need to be able to get up earlier, we need to be able to work harder. That same thing hurts your ability to actually be that person. And the brain is really interesting. Humans, everything about us is pretty interesting. But there’s a really pretty simple concept is if we’re low on gas, then it takes more horsepower. Or we get worse gas mileage in the things we need to do. And so if you run yourself dry, and then you expect to be a leader in a position where you’re not driven by ego, that’s going to be hard because you’re going to default to that because your brain’s going to think you are under some level of attack.
17:42
Podcast Host
So I love that you call that out because we do have to put the mask on ourselves first.
17:47
Kris Krustangel
It’s super hard to do again. I mean, we all live complex lives outside of work, I bet. So, you know, it’s hard to be that. But I would say that if I look back and I score myself right, the best work I’ve done, I’ve always done a better job of maintaining some self-investment along the way, you know, set calibration with the peers to get my mindset right, so then I can do the things I need to do both at home and at work to be successful. But again, I just want to say we’re all going to get off course, and it might be weeks, it might be months. Hopefully it’s just minutes. It’s just acknowledging where you’re at and trying to get practical about how to get back onto it.
18:21
Podcast Host
Kris, were you familiar with stoicism when you first kind of started this revelation around, hey, my ego’s in the way. I’m trying to look good. I’m trying to say the right things, but I’m talking right past the point that my superiors actually are asking me about. Were you familiar with stoicism at the time, or did you come across that along the way? And how did you interweave that into what you’re doing?
18:42
Kris Krustangel
I didn’t at the point. I mean, like a lot of things, it’s all just bravado and feeling early in the career. But, you know, I would say that there’s some input from my environment, my parents, my siblings. You know, you just kind of have a certain mind frame. But I didn’t understand it. Here’s what I did know. I did know that I had a growth mindset. I love to learn. I just do work, everything, random stuff. And it was like one of those things you get on a podcast, you listen to it, and they mention something, and you listen to another podcast and they mention the same thing. You’re like, wait a minute. I like these podcasts. They’re mentioning something, and then you dive into it.
19:12
Kris Krustangel
And so that probably happened, I would say, in the early 2012-2013, kind of just a couple years, 3, 4 years into my leadership roles, which I can’t believe was a decade ago, but, like, it was just the perfect time to then understand. The first off, we’re talking about thousands of years old, right? Philosophy. This isn’t decades. And just to hear that problems are still the same. I mean, from a societal standpoint, from a relational standpoint, they’re all still the same. And here’s these core tenets to help you better yourself as it relates to your environment, to deliver more value. And so then I kind of really dive in and I read the books, and I tend to go pretty deep, pretty quickly on the material, and then I come back up for air.
19:51
Kris Krustangel
And so now I just maintain what I would say is some refreshers, whether it be podcasts or blogs, et cetera, as well as just talking about it. I think we become better learners when we educate others about how it fits in foundationally in the work that we do, in the way that we act. So I wish I would have known it. I mean, I would have gone to it right after that meeting, you know, where my superior pulled me aside and said, you crapped the bed. But luckily, I stayed curious, and eventually I found the real pillars of the material to help me make it more clear in my head today.
20:21
Podcast Host
All right, so from a pure headcount perspective, there’s more sales reps in the organization, typically, than waiters, right. That’s just the way it is, and it’s an individual contributor role, and you’ve got a scoreboard, and the comp plans are set up for you to go. You go do. Ideally, if you’re winning, it’s good for the organization. If it’s a good comp plan, right. But it’s all about you driving your stuff. How do you talk to your team members? Or how do you advise people out there listening right now that are in that scenario? Or they’re only worried about their region because they want to make sure that their region isn’t the reason, say, maybe the country doesn’t hit right. How do they get out of that narrow lens? Or how do they marry that with the things that you’ve been discussing?
21:03
Podcast Host
Because that can be a challenge at times. You can be very tunnel focused and let everybody else worry about themselves or let the organization worry about what’s best. What’s your advice there?
21:12
Kris Krustangel
That’s an awesome question because I think about it a lot, you know, being fortunate. Like, I have to work across a couple organizations and work with some of the best reps I’ve ever seen in my career, up close and personal. There are two things that I like to convey to others. One is you kind of have to be a little selfish. And so I know I don’t want to contradict myself with the ego, but I think there has to be a certain sense of confidence and comfort in the plan or the approach or the knowledge that they have that maybe I don’t want to say average, but some of the parts rep may feel or look at things.
21:45
Kris Krustangel
And so it’s okay to challenge. It’s okay to feel passionate about how you’re gonna deliver success, because kind of that chip on the shoulder I always see is like, it’s like the gasoline in the engine. You can see this thing’s gonna go, it’s gonna fly. But the second thing that they do is really interesting. The best that I’ve seen, even though they may come off as, like, the funnest guy in the bar, gal in the bar, you know, they got the big energy, which I really do appreciate. I enjoy that, too. They’re very focused on delivering their success through other’s goals. Like, if you really ask them, if you really dig into them, they will tell you about their ten customers. They’ll tell you their whole lives, not just their personal stuff.
22:22
Kris Krustangel
They’ll tell you how they’re employed, how they care about patient flow, what the next board meeting is coming up. And they know all these really important motives to the physician and the physician supporters. And so what they’re doing is like, they’re providing that passion and that tenacity and that confidence, and they’re delivering success through what’s important to the customer, right? Regardless of what product, widget pill you sell. They are, like, locked into knowing in the most total version I’ve ever seen of all the information they could about what matters in that environment. And so kind of tying it back to the ego is the enemy: they’re not like, use my thing because I’m the greatest person ever. Even though some of them are just remarkable humans. Remarkable humans. They’re doing it because they know what they’re delivering…
23:08
Kris Krustangel
…helps all those motives and all those value drivers that the physician or the patient or the practice is looking for. And they may be obnoxious about it because maybe the physician doesn’t want to listen to them, but they will just, “I’m telling you, if you do x, we’ll get to y and you’ll be able to help, you know, this many more patients versus these patients.” Or if we do the procedures in the surgery center versus the hospital, look how that’s going to impact, you know, your work life balance. And it goes back to the idea again, the two things, having the passion and the tenacity and the confidence to know how to approach things, but then also having this just insisting, insane ability to analyze that opportunity and deliver success through the eyes of the customer and really value them.
23:48
Kris Krustangel
So that’s why I say it’s like, not ego driven. I mean, they’re utilizing the motives of others. And then they are the ones that are at peak club every year. They’re the ones that are making $500, 600, 700 million a year because they just, they know how to do that, and they have the passion to do it. I think it’s such an awesome question because it’s hard to do, and if it was easy, everybody would do it. But I think those two things just are none—and sorry to go a little long on this one—just separate the top of the top from everybody else. Those two things alone.
24:17
Podcast Host
So many visuals come to my mind when we’re talking about this and when we talk about in our business and asking questions. You need to understand not why someone should buy from you, but you need to understand what it is that impacts them about what you can bring to the table. It’s just like if you’re walking by and someone’s trying to cook the most delicious dish on the planet, and you can go sprinkle the perfect thing. Like, there’s no ego in that. If it turned that into the most delicious. But you need to understand the dish and you need to understand what flavor they think is delicious. Because you might think that ice cream is delicious, but if they’re cooking eggs and broccoli, well, probably not a good fit.
25:01
Podcast Host
So I love that you called that out, because I get really geeked out about this because basically what you’re talking about is you’re talking about constraint theory as it relates to behavior and decision making. Within surgeons or physicians who have been taught a very specific thing, they have a bounded rationality, a bounded knowledge of what they’re doing, which makes it hard for them to recognize how powerful your tool could be. And when you are non-ego driven, you can understand their perspective and come in and sprinkle in that perfect ingredient. I love how you just broke that down. That is every rep who just heard that. You need to go check yourself against that description. That was awesome.
25:47
Kris Krustangel
Yeah. And I appreciate it’s hard, again, and if you’re not willing to do that, the hard work, it’s not going to happen at the same level. You can still have success, right, with a few customers, et cetera. But if you’re not really going to dig in like we just discussed and deliver on a different level, you’re not going to be the person who sustains three, four, or five years of just high earnings, high impact factor potential. It’s just not going to work. And I just want to say one thing. There’s a nuance, what you just said about the constraint theory that we don’t talk about a ton generally. Like, I actually haven’t heard that in a while. But just think about how physician is trained, right. It’s all protocol, workflow based, UCX, UGY, etc. And I’m not trying to minimize for any physicians listening.
26:22
Kris Krustangel
I realize you’re far more dynamic than that, but generally you’re given a set of blueprints to kind of follow. The challenge—and I would argue being a frontline physician is where the hardest jobs are—is because: “Yeah, that’s great when I was taught it, and these are all therapies that I had.” Fast forward five or ten years with the dynamic shift of the payor, the dynamic shift of new entrants, the dynamic shift of reps, and so all of that is changing at incredibly rapid speed. But what’s the same? The physician still wants to do something. They still want to get something done for themselves or for their practice, for their patients. None of that has changed.
26:56
Kris Krustangel
So if you can come in as a rep and understand all those pieces of information they’re trying to sort through, all the things that they care about, then you see it more clearly than them sometimes and be like, oh, hey, it’s just this. Let’s do this one thing. And again, it’s not easy. It’s certainly not easy. It’s not for those that want to go fast, but it’s for those who want to set up long term success and create meaningful value, which I want to point out too oftentimes that the top reps, I think, get mislabeled as, you know, they just want to make a bunch of money. If you sit with and talk to them, that’s just like a part of it. They want to be meaningful. They want to help patients. They really want to help physicians.
27:32
Kris Krustangel
And they are more wound up passionately about that than even I am. You can sense I’m pretty passionate about it. Like, they want to drive impact. And so you got to remember that, too. In addition to the practical things we just talked about. You got to really want to help. You got to really want to help other people and mean it, and if you can put all those things together, back to, you know, your recipe, it’s going to taste amazing. And you’re going to have a ton of success, and people are going to be back for more, for sure.
27:58
Podcast Host
I probably shouldn’t mention it because I can’t even find it, but when I was looking down, I was trying to find, there’s a term that actually Matthew McConaughey has in his book Green Lights, because we throw a ton of books out there today, that literally describes this. I can’t remember what it’s called. I couldn’t find it.
28:10
Podcast Host
So we’ll have to drag it down and put it here.
28:12
Podcast Host
Yeah, we will.
28:13
Kris Krustangel
You have to get Matthew McConaughey on next.
28:15
Podcast Host
Yeah, there we go. But I love the description of it because it’s literally, it’s like, no, be selfish, but use the selfishness for the good of others around you. And that’s what you’re describing, right? Totally. To think that we’re not selfish or that you’re not out for your own interest is foolish because that’s part of our human nature. But just like the cell phone was amazing invention, right, piece of technology. It can be used for amazing things, like connecting us to our parents that don’t live here, you know, close to us with FaceTime, or to do something nefarious like set up a bomb somewhere. It’s all about how you leverage it. So I think that’s what the essence of what you were describing, and I wish I could come up with that term. I couldn’t find it.
28:52
Kris Krustangel
But you’re gonna find it an hour from now.
28:53
Podcast Host
That’s a great point. I’m glad you tied those two things together, too.
28:56
Podcast Host
That is awesome, Kris. I really appreciate you taking the time and spending it with us today. This has been a great episode. There’s so many little nuggets that people can take away and help with their own growth. We’ll put links to the books you mentioned, Ego is the Enemy and The Obstacle is the Way. I would second, and I’m sure Clark would third the recommendation on consuming those books 100%. We actually, just as a side note, because it was such an important book to me, The Obstacle is the Way is read by every employee in our organization when they onboard. So really appreciate it. If people want to connect with you, chat, ask questions, is it okay if they reach out to you through LinkedIn?
29:37
Kris Krustangel
Yep. That’s probably my best medium. I tend to try to be pretty active, both for the greater good of just our community, as well as just talking about what I do and what the products we sell do for the patients we work with.