Many providers are moving beyond epidural steroid injections (ESIs) for patients with chronic low back pain associated with lumbar spinal stenosis (LSS).
Instead of simply masking the pain caused by an enlarged ligament with epidural injections, which may only provide temporary pain relief, providers now opt for more innovative and durable spinal stenosis treatment options such as the mild® Procedure.
An epidural steroid injection, which is a medication that is injected into the epidural space in the lower spine to reduce swelling and offer pain relief, may be offered to patients with chronic low back pain from conditions such as lumbar spinal stenosis.
Recent data indicates that repeat epidural injections for patients who experience only short-term improvement may not be in the patient’s best interest in the long term. Alternative treatments, such as minimally invasive lumbar decompression, or the mild® Procedure, may be a better option for some patients.
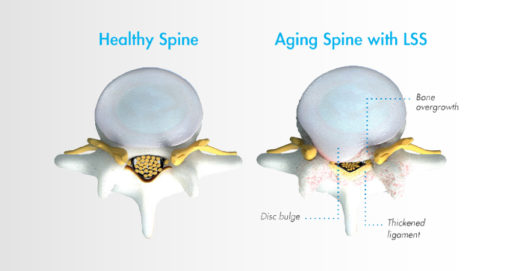
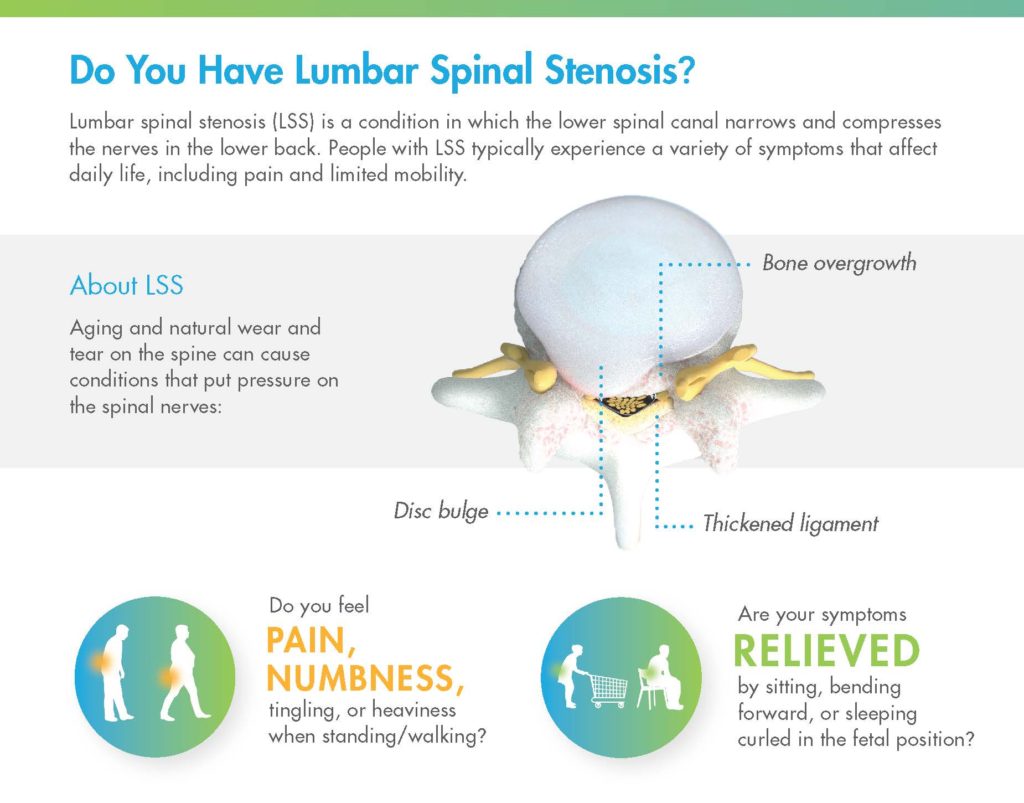
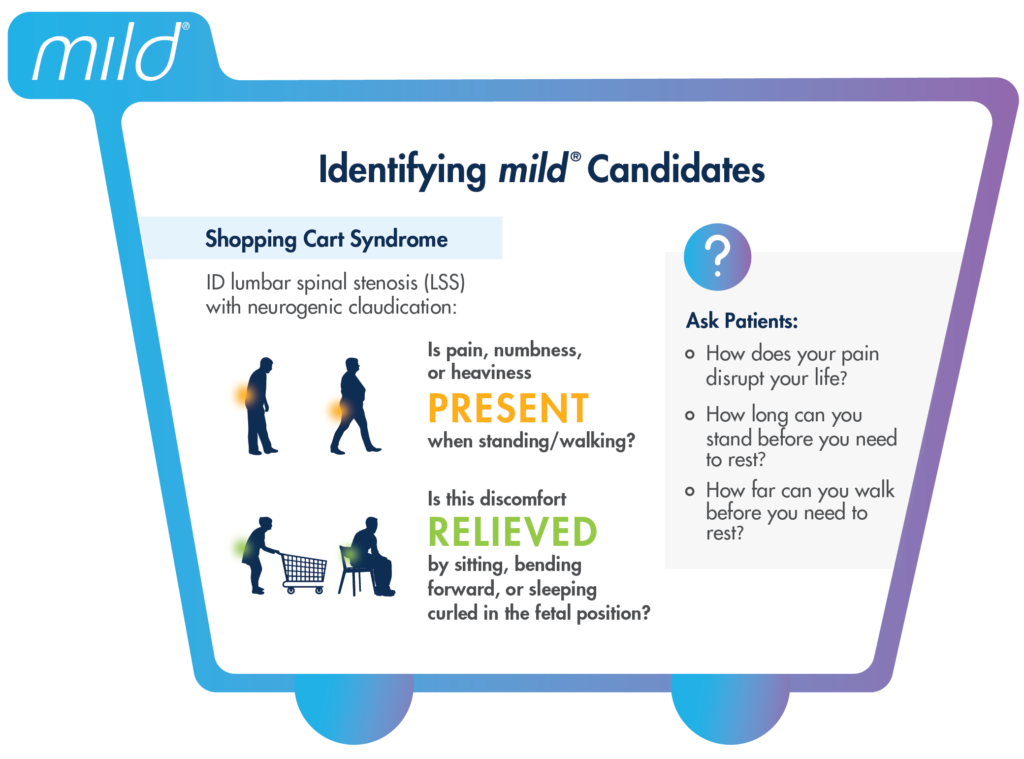
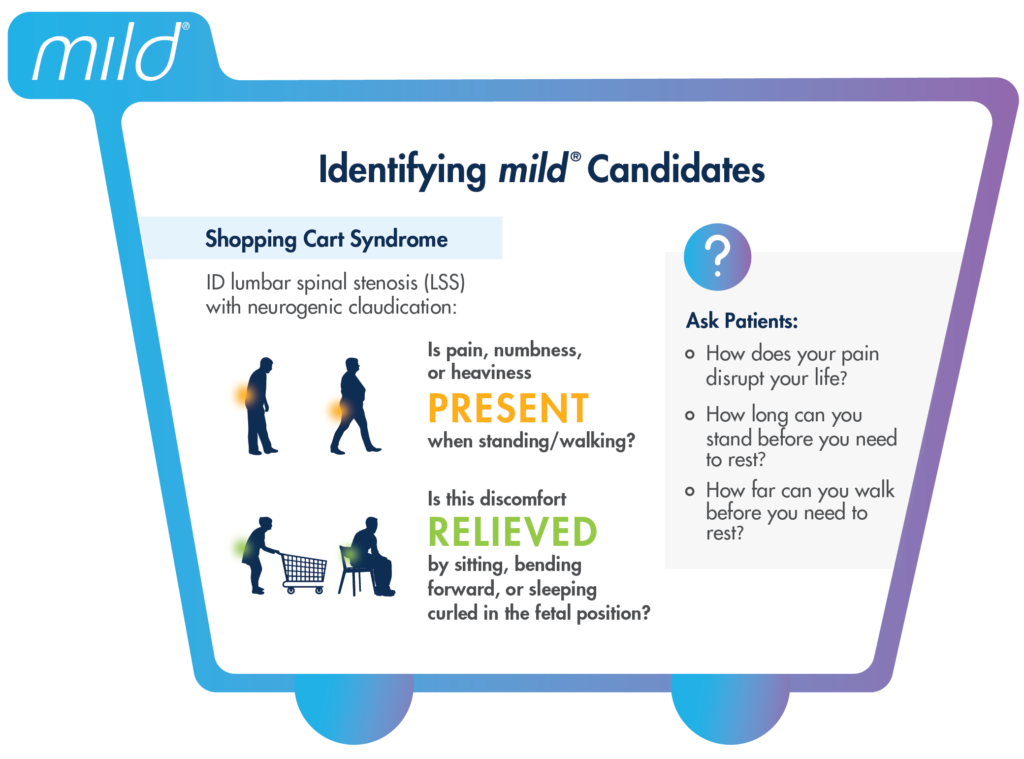
Lumbar spinal stenosis, also called LSS, contributes to chronic low back pain and is prevalent in approximately 20 percent of patients over the age of 60. LSS is often caused by an enlarged ligament in the back, which compresses the space around the spinal canal and puts pressure on the nerves in the lower back. This pressure around the spinal cord can cause pain, numbness, heaviness, or tingling in the low back, legs, and buttocks. A common visual cue is often referred to as the “shopping cart syndrome,” where the act of leaning over, often over a shopping cart, cane, or walker, helps to temporarily alleviate pressure felt in the lower back pain.
In addition to epidural steroid injections, some common conservative treatment options for LSS can include the mild® Procedure, medication, and/or physical therapy, with more invasive options including procedures such as spacer implants, spinal stenosis surgery, or other open surgery.
Epidural steroid injections are typically offered to LSS patients when more conservative treatment options, such as exercise and physical therapy, have failed to provide relief.
Steroid medication is injected directly into the epidural space, which may relieve pain by reducing inflammation around the spinal cord and nerves. The effects typically last for less than 6 months, after which additional injections may need to be administered.
Data shows that epidural steroid injections can effectively relieve pain for LSS patients—but the effects are not lasting, and pain may return, typically in months. ESIs treat the symptoms but do not address the root cause of pain associated with LSS.
While ESIs are an effective form of early treatment for some patients, they may not provide reliable, lasting relief for all low back pain.
As mentioned in the Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST), certain payer guidelines, including Centers for Medicare and Medicaid Services (CMS), now stipulate that patients should have obtained a minimum of 3 months of pain relief with eventual recurrence of pain before it is reasonable to proceed with additional injection therapy.
This means that for patients exhibiting shorter-term relief of less than 3 months after receiving an ESI, clinicians should consider alternative treatment options.
Steroid medication reduces inflammation, which can temporarily relieve pain. However, epidural steroid injections only treat the symptoms of LSS—not the root causes of pain and inflammation. The effects of epidural steroid injections typically last less than 6 months, and patients often require an average of 2–3 injections per year to sustain long-term relief from low back pain associated with LSS.
There are many patients for whom repeat epidural steroid injections may offer more risks than benefits. For instance, steroid medications have been linked to bone loss, or osteoporosis. ESIs may also introduce risks for patients with certain comorbidities such as diabetes, cardiovascular conditions, active infections, bleeding disorders, or those taking anticoagulant medications.
As an alternative, epidural injections without the use of steroids may be considered, as well as more advanced decompressive therapies such as the mild® Procedure.
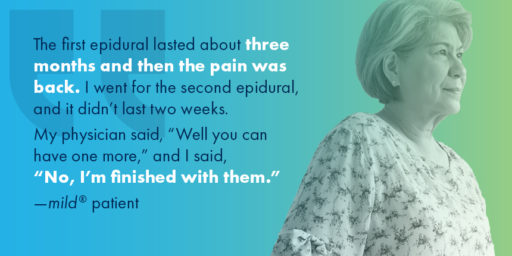
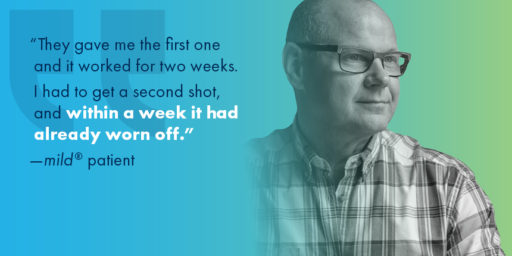
In addition to the health concerns associated with repeat steroid injections, the mental and emotional effects experienced by many LSS patients can also reveal the dark side of repeat epidural steroid injection treatments.
Due to the temporary nature of epidural steroid injection relief and the requirement for repeat injections, many practices encounter patients with what is increasingly becoming known as “ESI Exhaustion.” ESI Exhaustion can be spotted in patients at any stage of LSS treatment or stenosis severity.
When patients experience short-term relief for a condition as challenging as LSS, they can easily become frustrated and lose hope. LSS patients often experience debilitating pain and loss of mobility that can have a devastating impact on their outlook and optimism for the future. Losing additional time and energy to repeated appointments, procedures, and recovery times can also be detrimental to their quality of life, and some patients may start to feel hopeless if injections remain ineffective or lose their efficacy soon after receiving them.
One of the more common questions patients have about a steroid injection is, “How long will the results last?” Unfortunately, with epidural steroid injections, efficacy can vary by patient, and it can be difficult to predict the degree of relief or durability of effect for the individual. While studies have shown symptom relief for up to 6 months in some lumbar spinal stenosis patients, other studies have demonstrated the limited effectiveness of epidural steroid injections.
If patients are dissatisfied with their results and feel they have run out of options in your practice, they may search for another solution. By offering alternative treatments such as the mild® Procedure as an early intervention, you can retain the patients in your practice and increase productivity, while continuing to develop closer relationships and increase your reach within your community.
Given the significant advances in minimally invasive spine technology, current research confirms that repeat epidural steroid injections should be reserved only for patients who experience significant and lasting relief after the injections, and/or those who are not candidates for higher-level interventions or surgical decompression.
For patients experiencing relief that lasts fewer than 3 months, clinicians may wish to consider more durable treatment options.
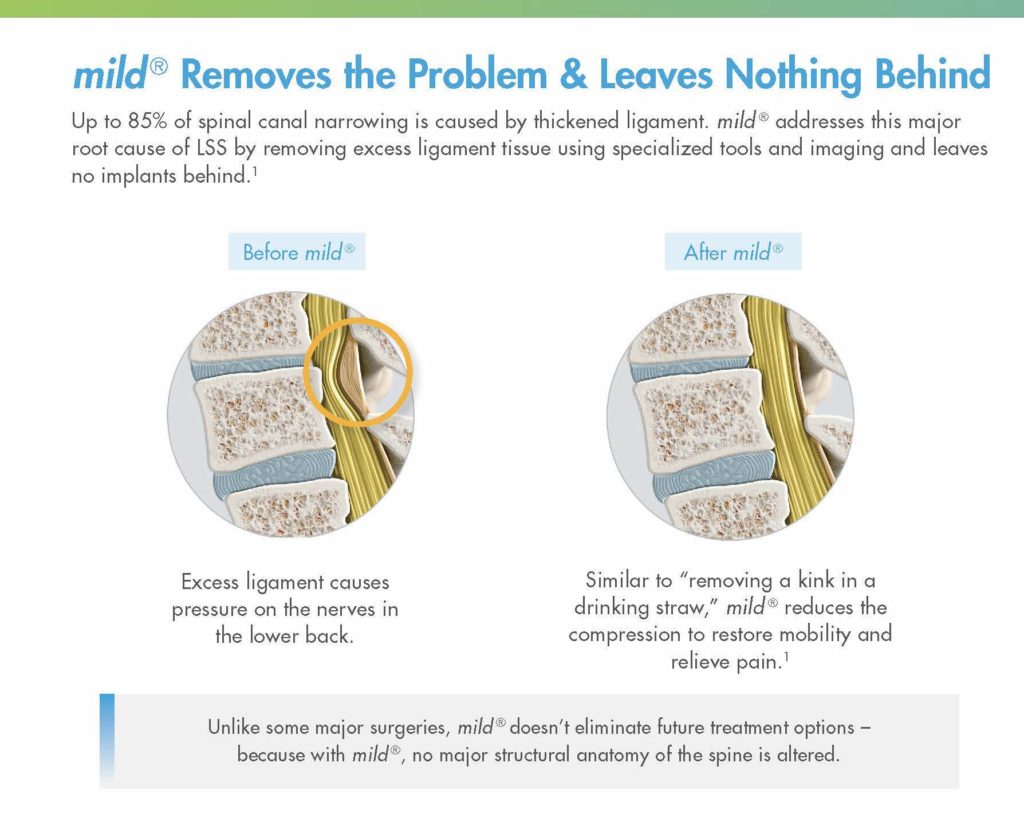
While they may offer temporary relief, epidural steroid injections do not “cure” LSS. Without addressing the enlarged ligament, which contributes up to 85% of spinal canal narrowing , relief may only be experienced on a short-term or temporary basis.
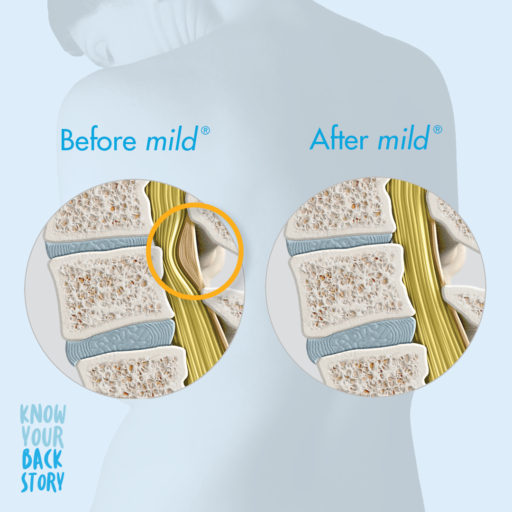
Minimally invasive lumbar decompression may be the next step for long-lasting relief from LSS and to reduce pressure in the canal. By decreasing the amount of space taken up by the enlarged ligament, patients can experience decreased pressure on the spinal nerves, which may lead to decreased pain.
Performing multiple epidural steroid injections only delays patients from receiving treatment with more lasting results, such as minimally invasive lumbar decompression—the mild® Procedure.
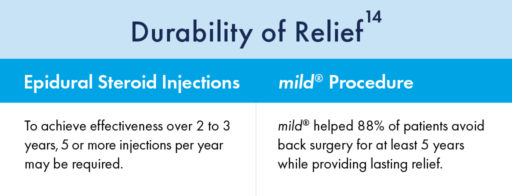
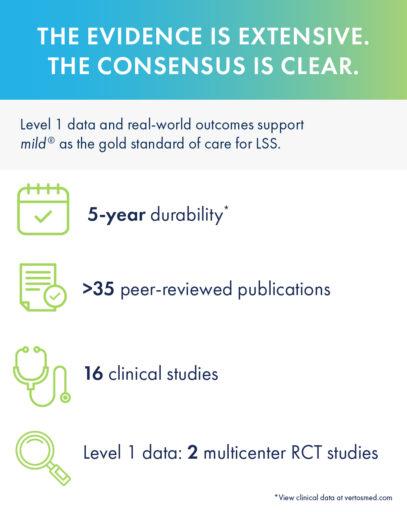
Turning to mild® as the first line of therapy addresses the root cause of LSS by removing excess ligament tissue around the spine, proven to provide a 5-year durability of results.
The mild® Procedure is a short, outpatient procedure that can be performed using only local anesthetic and light sedation. The procedure is performed through a single incision in the low back smaller than the size of a baby aspirin, or the diameter of a drinking straw (5.1mm).
By removing excess ligament tissue that has built up around the spine, mild® restores space in the spinal canal. This reduces pressure on the nerves in the low back, addressing a major root cause of LSS, which can help reduce pain.

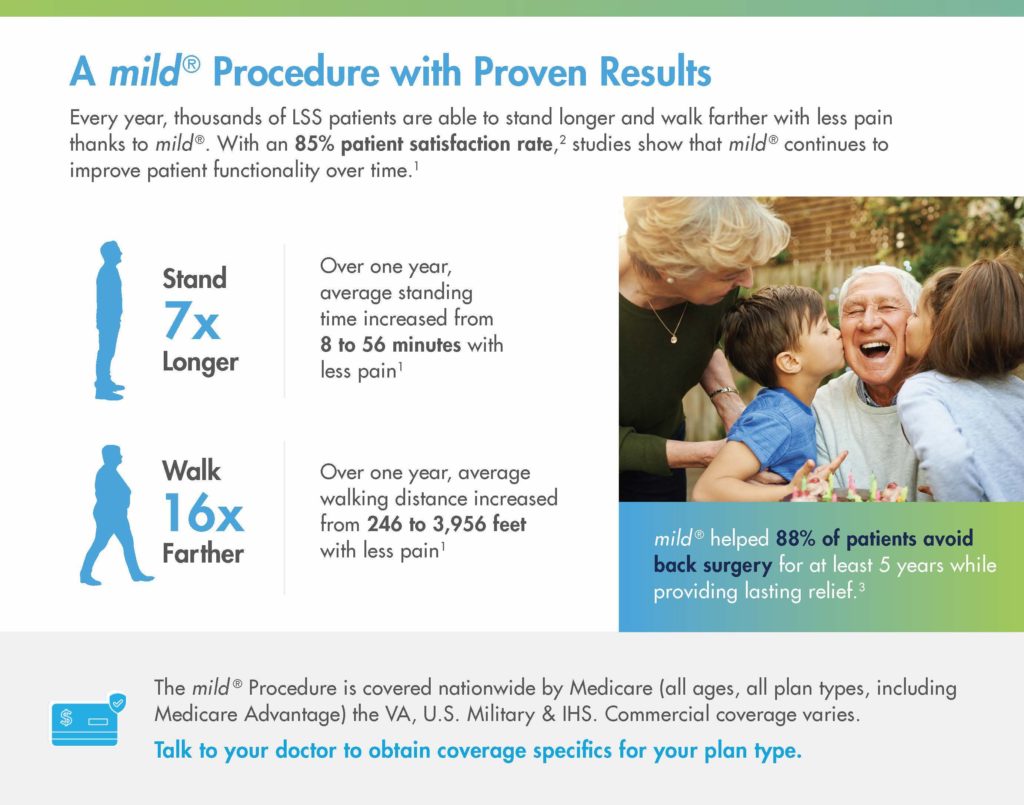
When Epidural Steroid Injections (ESIs) Don’t Provide Lasting Relief, mild® can improve patient outcomes across a variety of measures:
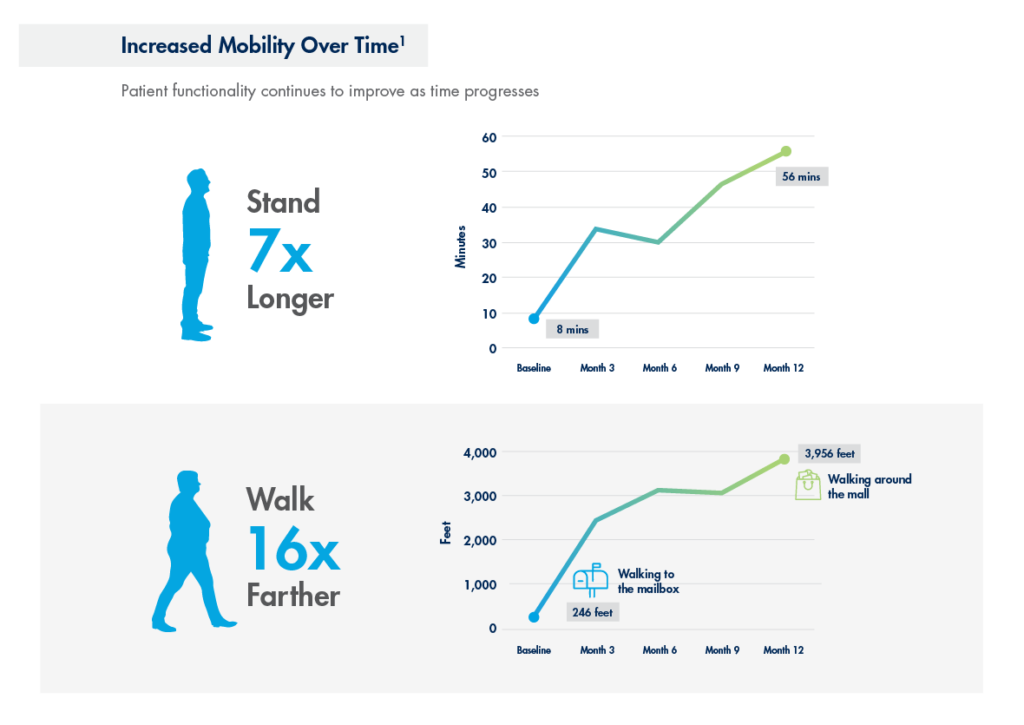
In a study performed at the Cleveland Clinic 1 year after the mild® Procedure, patients were able to:
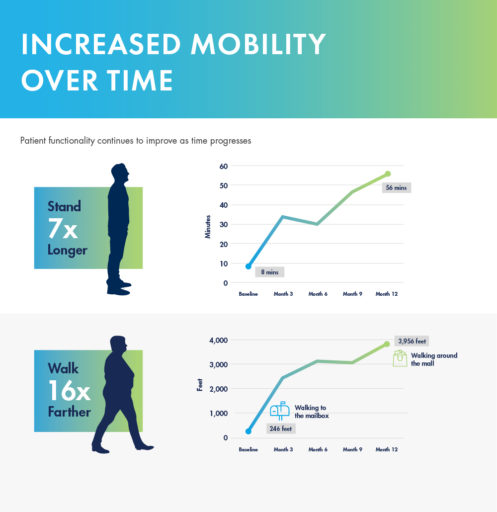
mild® demonstrated excellent long-term durability with significant improvements in both pain and mobility over 2 years. Clinical data from the MiDAS ENCORE 2-Year Study finds mild® provided patients with lasting pain relief and increased mobility.
A 5-year study performed at the Cleveland Clinic demonstrated that mild® helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief. Use our Find a mild® Doctor tool to connect with an interventional pain management specialist in your local area to find out if mild® is right for you.
To learn more about mild® and how it can help people suffering from LSS get on the path to lasting relief, explore mildprocedure.com.
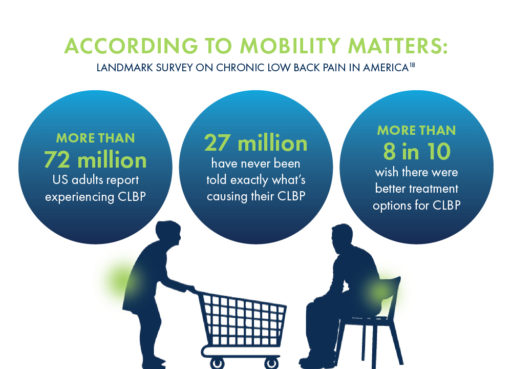
Vertos Medical is proud to have joined forces with the American Society of Pain & Neuroscience (ASPN) and the National Association of Memoir Writers (NAMW) to develop the Know Your Back Story campaign, a national public health awareness campaign that seeks to help patients suffering from chronic low back pain (CLBP) learn more about their “back stories.” The campaign encourages providers to educate their patients on lumbar spinal stenosis (LSS) and provide awareness around the enlarged ligament that may be causing their pain.
Vertos Medical is committed to empowering healthcare providers and patients with minimally invasive treatments for LSS, and the Know Your Back Story campaign plays a significant role in fulfilling our core mission: to help patients suffering from chronic back pain reclaim their quality of life using the simplest, safest, most durable, and earliest treatment available.
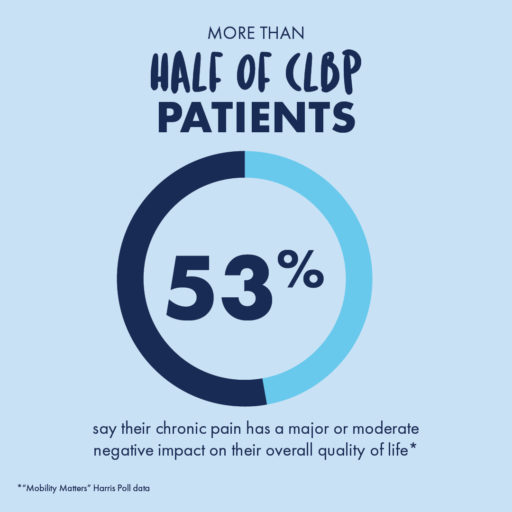
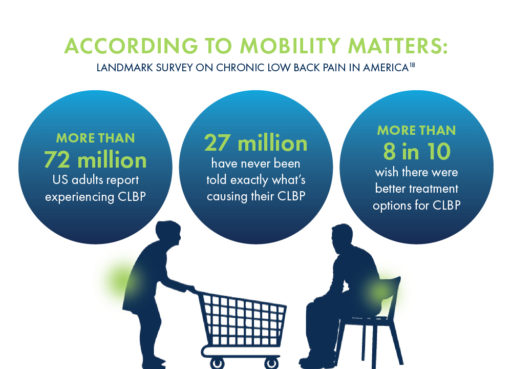
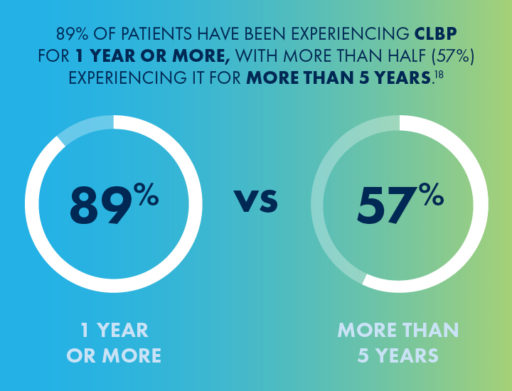
As part of the Know Your Back Story campaign, we partnered with The Harris Poll to conduct a landmark survey on CLBP in the United States. Results from the “Mobility Matters: Chronic Low Back Pain in America” survey indicate that CLBP affects more people than arthritis, diabetes, or heart disease, but over one-third of CLBP patients have never been told by a provider what the exact cause of their pain is.
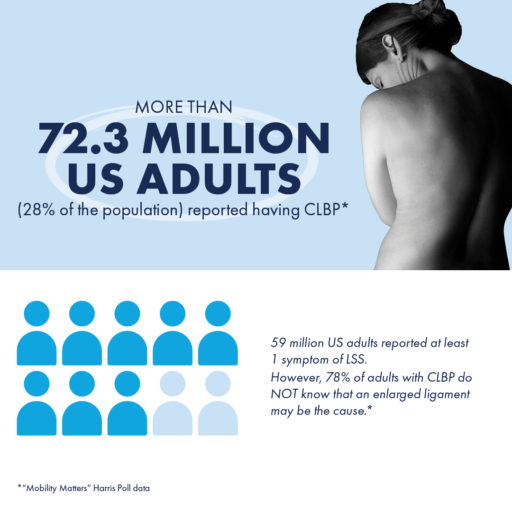
“Mobility Matters: Landmark Survey on Chronic Low Back Pain in America” also revealed misconceptions about CLBP and the need for education about the associated impacts on mobility and quality of life, and where to go to for diagnoses and information about available treatment options.
The average chronic low back pain sufferer has seen at least 3 different healthcare professionals (HCPs) seeking treatment for their pain and has made 4 visits to an HCP within the last year.
For the most accurate diagnoses and treatment recommendations that may lead to lasting relief, patients should seek out doctors who specialize in spine health, such as pain specialists, physical medicine, and rehabilitation (PM&R) physicians, interventional pain physicians, or physiatrists.
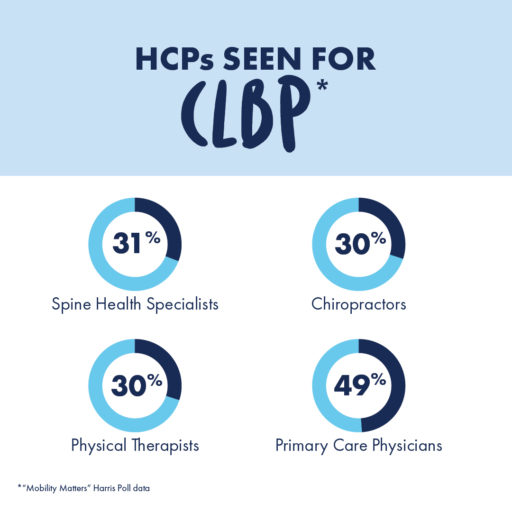
By meeting with doctors who specialize in spine health, patients may be able to gain new insights into the root cause of their pain.
Lumbar spinal stenosis (LSS) is a condition, prevalent in approximately 20% of patients over the age of 60, in which the lower spinal canal narrows and compresses the nerves in the lower back. Up to 85% of spinal canal narrowing is caused by an enlarged ligament.
This pressure around the spinal cord can cause pain, numbness, heaviness, or tingling in the low back, legs, and buttocks, but the vast majority of CLBP patients have never heard of this potential diagnosis.
The Know Your Back Story campaign’s objective is to spread awareness around LSS and get more patients on the path to lasting relief. By collecting intensive data, developing tools for patient education, and sharing insights with both patients and providers about the effects of LSS and its potential treatment options, the Know Your Back Story campaign has served as a significant step in bringing more visibility to this condition.
Getting screened for LSS and CLBP can open the door to learning more about treatment options available, such as the mild® Procedure.
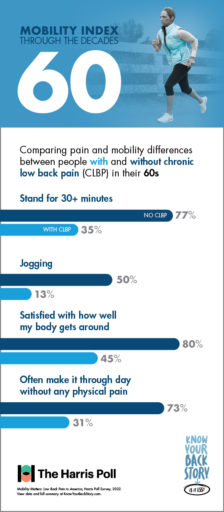
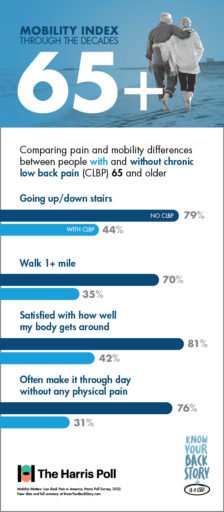
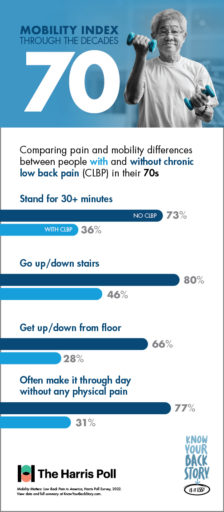
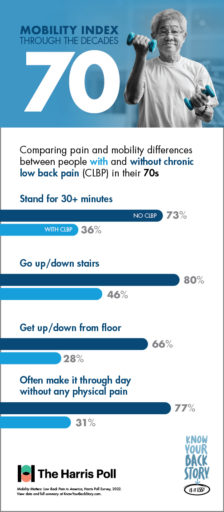
One of the key accomplishments of the Know Your Back Story campaign is the development of the first-ever Mobility Index, a breakthrough resource for demonstrating the differences in mobility and quality of life between patients with CLBP and their peers without CLBP.
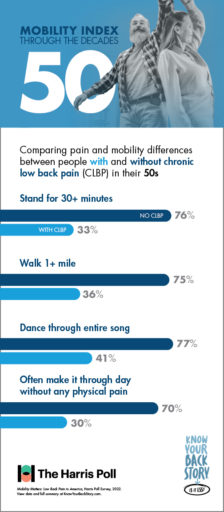
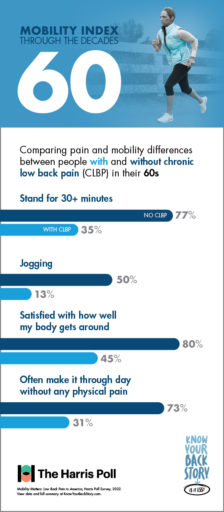
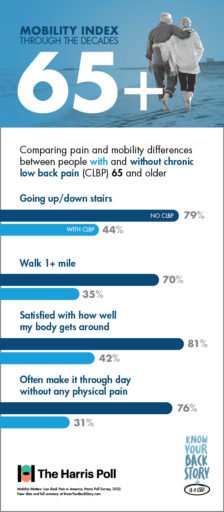
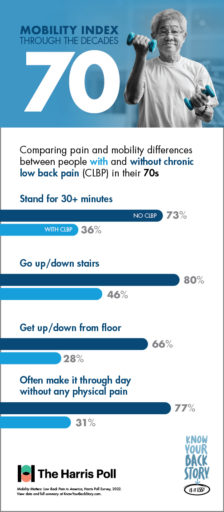
Results from the “Mobility Matters: Landmark Survey on Chronic Low Back Pain in America” conducted by The Harris Poll show that with age, CLBP patients experience significantly greater challenges performing physical tasks and making it through the day without pain or limited mobility than others within their age group without low back pain.
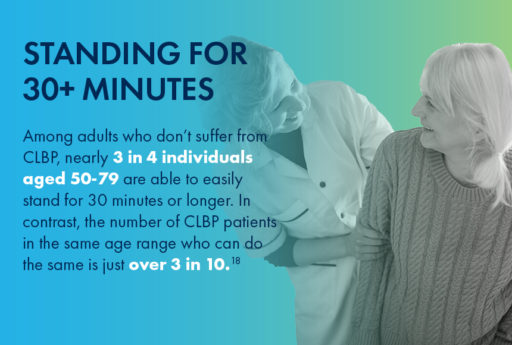
For instance, nearly 3 in 4 individuals in their 50s who do not suffer from CLBP are able to easily stand for half an hour or longer. In contrast, the number of CLBP patients in the same age range who are able to do the same is just over 3 in 10.
When it comes to other activities such as walking, dancing, or using the stairs, the Mobility Index can be a great tool for educating patients. By reviewing the differences in mobility between similar individuals with and without CLBP, patients can understand more about what chronic pain is keeping them from—and their options for finding lasting relief.
On the quest to educate, engage, and increase awareness within communities, the Know Your Back Story campaign took the #LookForTheLigament Education and Experiential Mobile Unit on tour down the East Coast, stopping in New York City, NY; Philadelphia, PA; Washington, D.C.; and Sarasota, West Palm Beach, and Miami, FL.
The mission of this tour was to encourage people suffering from CLBP to get screened for LSS and an enlarged ligament by a spine health doctor, and to provide both patients and HCPs with an in-depth look at the causes and effects of LSS through interactive experiences and demonstrations, including:
By staying aware of the impacts of LSS and CLBP on patients’ mobility and potential treatment options, healthcare providers can help more patients in their communities get on the path to lasting relief. By working alongside others in their practice or by creating referral networks with primary care, physical therapy providers, and other local providers, HCPs in Interventional Pain Management (IPM) or spine health specialties can play a more effective role in identifying patients suffering with LSS or CLBP and connect them to providers that are able to offer more durable treatment options.
Physicians and Advanced Practice Providers (APPs) can also play a more proactive role in identifying LSS by staying aware of common patient misconceptions about back pain. By utilizing the tools and resources developed as part of the Know Your Back Story campaign, you can keep your patients as educated as possible about the potential causes of their chronic pain, as well as the treatment options that may finally provide them with relief.
For patients looking to learn more about the source of their pain and their options for relief, finding a local spine health doctor is a crucial first step. By using the MD Finder tool, patients can find doctors in their area who may be able to provide the answers they’ve been seeking.
A spine health specialist can help walk patients through their options for treatment, from more conservative therapies such as medication or physical therapy to longer lasting, minimally invasive treatments such as the mild® Procedure.
The mild® Procedure, or minimally invasive lumbar decompression, may be pursued as a first-line therapy for LSS.
A minimally invasive procedure that is considered the gold standard of care in LSS treatment, mild® addresses a major root cause of LSS by debulking the enlarged ligament to restore space in the spinal canal and reduce compression of the nerves. With a safety profile equivalent to an epidural steroid injection (ESI), mild® has helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief,—a durable, lower-risk treatment option to spacer implants or open surgery.

For patients considering mild®, the Move More Questionnaire is a great resource for identifying current limitations and tracking their reduced pain and improved mobility after the procedure.
By becoming familiar with the Know Your Back Story campaign and exploring the insights and resources developed to spread awareness about LSS, both patients and providers can help spread the word about this under-diagnosed cause of CLBP.
Vertos Medical is committed to helping patients experiencing chronic pain reclaim their quality of life with a short, minimally invasive early treatment option with the mild® Procedure, both through the Know Your Back Story campaign and in everything we do.
If you experience chronic low back pain (CLBP), you may have questions: What’s causing it? What do my symptoms mean? Will my condition worsen as I age? How can I find relief?
You’re looking for answers—and you’re not alone. Unlike other debilitating conditions, researchers have never truly known how many people suffer from CLBP. Until recently, many patients have been left in the dark about the cause of their pain or their options for treatment.
As revealed in the Mobility Matters: Landmark Survey on Chronic Low Back Pain in America, created in partnership with The Harris Poll, there are many misconceptions about chronic low back pain, including its potential causes, symptoms, and treatment options.
Before this survey, we didn’t know which patients were suffering the most, or how the CLBP experience may change through life’s decades. In this blog, we’ll share the results of the survey, explore a common, yet often undiagnosed, cause of CLBP, and discuss some of the treatment options available for patients seeking relief.
As we grow older, it can be difficult to assess which mobility challenges are a normal part of aging, and which ones may indicate a condition such as CLBP. The Mobility Index, developed as part of the national Know Your Back Story campaign, was designed to demonstrate how older adults could be moving through life if chronic low back or leg pain was not a limiting factor.
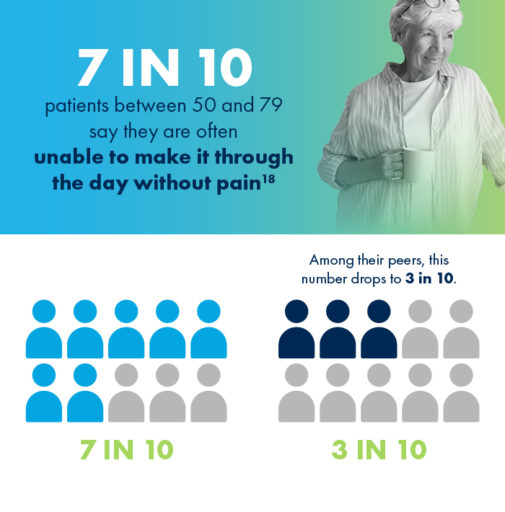
Poll results show that with age, CLBP patients experience significantly greater challenges performing physical tasks and making it through the day without pain than their peers who do not suffer from low back pain.
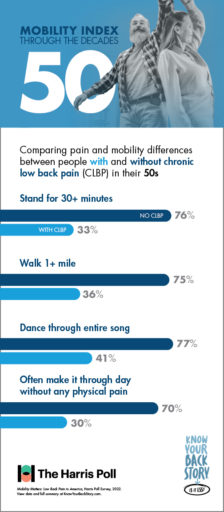
If you’re suffering from CLBP, you’re already familiar with the limits your pain can put on daily tasks and activities. But do you know just how much you could be doing without these obstacles?
For CLBP patients in their 50s, having difficulty doing physical activities that were once a regular part of life, such as walking a mile or dancing for the duration of one song, can feel especially discouraging.

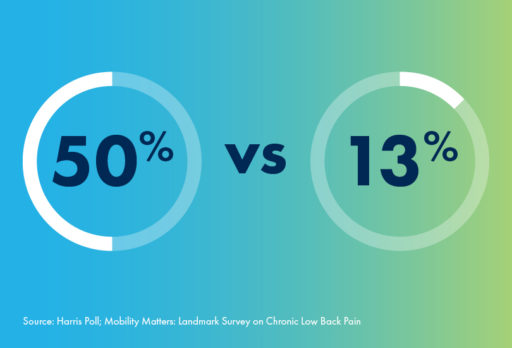
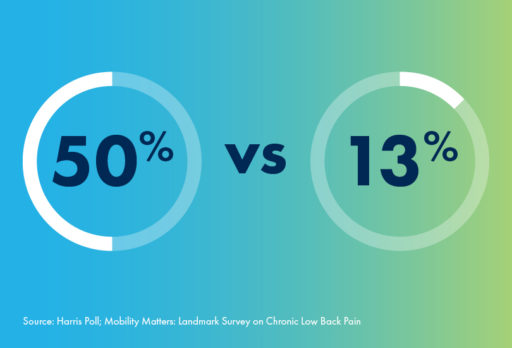
For people in their 60s, there are some activities like—jogging—that aren’t for everyone. Even among individuals without CLBP, only 50% of respondents in their 60s reported the ability to jog with ease. However, for patients suffering with chronic low back pain, this number plummets to only 13%.
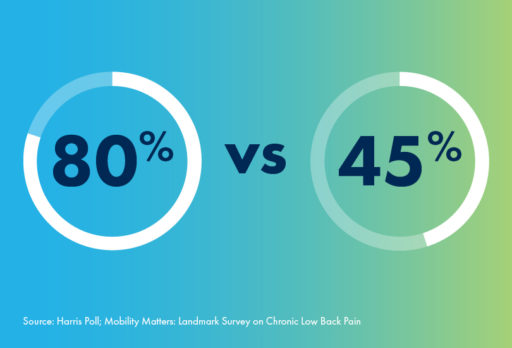
And whether jogging, walking, or doing anything else, fewer than half of CLBP patients in their 60s say they feel satisfied with how their body gets around. In contrast, 80% of 60-somethings without CLBP are satisfied with their mobility.
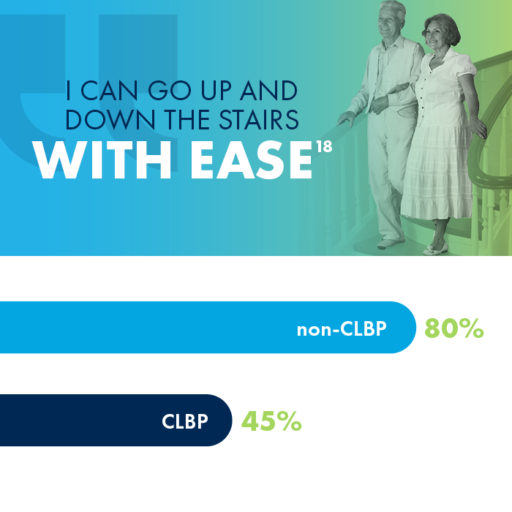
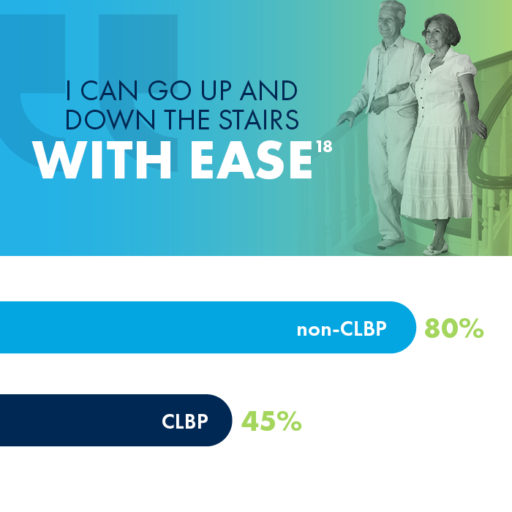
Did you know that 80% of people in their 70s without CLBP are able to easily go up and down the stairs? If you are a CLBP sufferer in your 70s, you may have a much different experience, as fewer than half of CLBP patients in their 70s reported the same mobility using stairs.
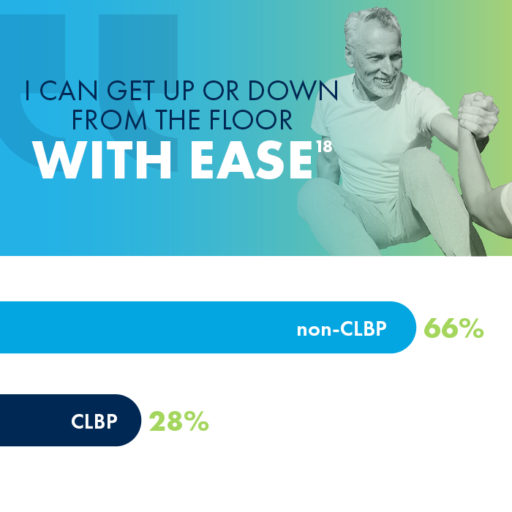
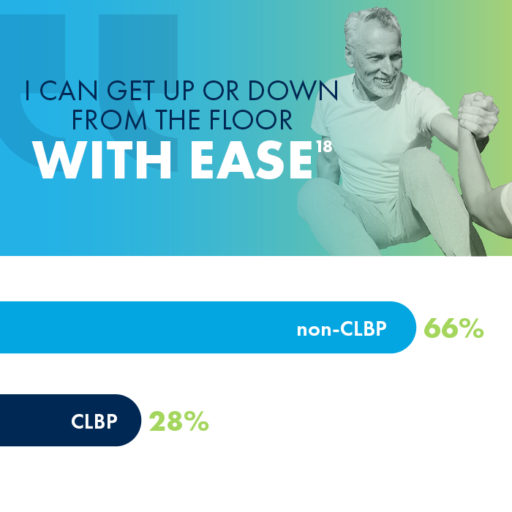
Getting up from the floor is another activity that impacts CLBP sufferers much more than their peers who don’t experience chronic pain. While 66% of 70-somethings without CLBP reported ease in getting up or down from the floor, only 28% of those with CLBP were able to say the same.

One cause of low back pain that often goes undiagnosed is an enlarged ligament, which can contribute to lumbar spinal stenosis (LSS), a common, yet overlooked, condition that millions of people may be unaware of.
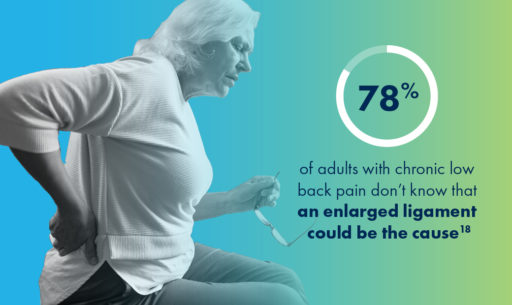
Lumbar spinal stenosis (LSS) is a common, yet overlooked, condition that is prevalent in nearly 20% of patients over the age of 60.
LSS is often caused by an enlarged ligament in the back, which compresses the space in the spinal canal and puts pressure on the nerves in the lower back. This pressure around the spinal cord can cause pain, numbness, heaviness, or tingling in the low back, legs, and buttocks.
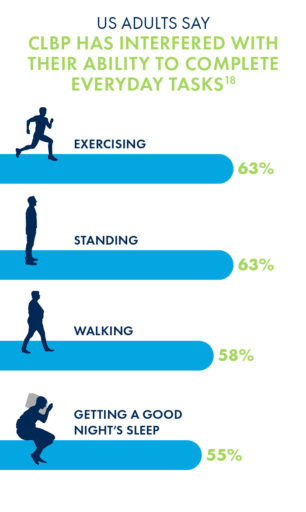
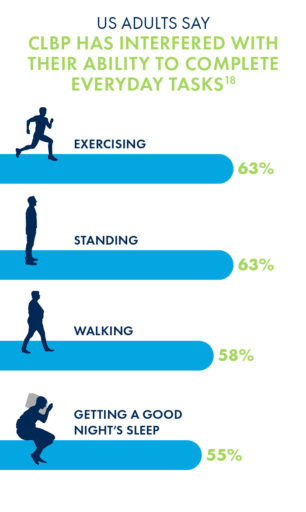
Unsurprisingly, the chronic low back pain that may be caused by LSS has negative impacts on nearly every aspect of a patient’s life, most commonly in their abilities to exercise, stand or walk for long periods of time, and get a good night’s sleep.
Due to its minimally invasive nature and long-lasting durability, many interventional pain management doctors are making the move to mild® as an alternative to epidural steroid injections (ESIs), which may only work in the short-term and may require repeat injections to maintain relief.
More invasive courses of treatment can include procedures such as spacer implants or open surgery, though nearly 80% of CLBP sufferers have concerns about undergoing surgery.
The mild® Procedure, or minimally invasive lumbar decompression, is considered a gold standard of care among treatments for low back pain. By addressing the root cause of pain, the enlarged ligament, mild® has helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief.
When patients present complaining of chronic low back pain (CLBP), they’re relying on you, as their provider, to help them find answers. Many patients want to know what’s causing their pain, how their condition will progress over time, and perhaps most importantly, how they can find relief.
As revealed in the Mobility Matters: Landmark Survey on Chronic Low Back Pain in America, created in partnership with The Harris Poll, many CLBP patients feel that they have been left in the dark about the cause of their pain or their options for treatment; as a provider, you’re all too familiar with the challenges and frustrations that can come with chronic pain.
In this blog, we’ll share some of the results of the groundbreaking survey, including new insights into how CLBP can impact patients’ lives as they age. We’ll also explore a common, though often undiagnosed, cause of CLBP and discuss some of the treatment options available for patients seeking relief.
By staying informed about the causes of low back pain, educating patients about their treatment options, and encouraging patients to seek help from spine health specialists, healthcare providers can play a key role in improving patients’ quality of life.
One cause of CLBP that often goes undiagnosed is an enlarged ligament in the lower back, which can contribute to lumbar spinal stenosis (LSS). LSS is a common, yet overlooked, condition that is prevalent in nearly 20% of patients over the age of 60.
LSS is often caused by an enlarged ligament in the back, which compresses the space in the spinal canal and puts pressure on the nerves in the lower back. This pressure around the spinal cord can cause pain, numbness, heaviness, or tingling in the low back, legs, and buttocks.
By recognizing the symptoms and understanding the treatment options, you may be able to identify the condition sooner in your patients with chronic low back pain and get them on the path to lasting relief.

Unsurprisingly, CLBP that may be caused by LSS has negative impacts on nearly every aspect of a patient’s life—most commonly in the ability to exercise, stand or walk for long periods of time, or get a good night’s sleep.
As patients age, it can be difficult to assess which mobility challenges are a normal part of aging, and which may have an explanation, such as an enlarged ligament.
The Mobility Index was designed to demonstrate just how different life could be for older adults if chronic low back or leg pain was not a limiting factor.
Results from the Mobility Matters survey indicate that adults with CLBP face significantly more difficulties performing physical activity and making it through the day without pain than their peers without chronic pain.
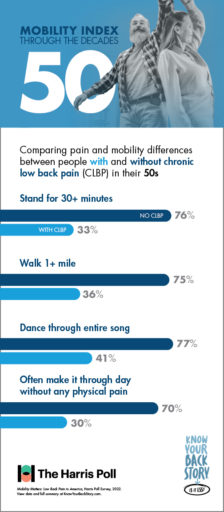
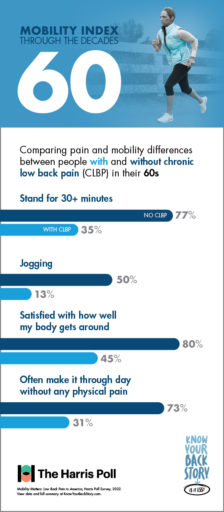
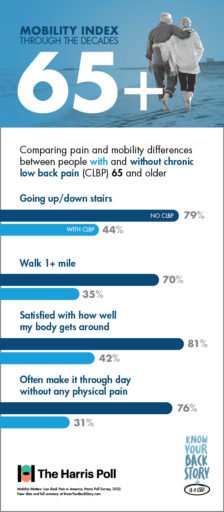
Patients who suffer from CLBP are already familiar with the limits their pain can put on carrying out daily tasks and activities. But they may not even realize just how much they’re missing out.
When it comes to activities such as walking, dancing, using the stairs, and more, the Mobility Index can be a great tool for educating patients. By reviewing the differences in mobility between individuals with and without CLBP, you can help your patients understand more about their mobility and their options for relief.
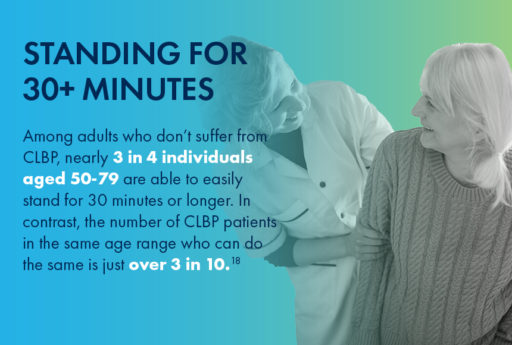
For CLBP patients in their 50s, having difficulty doing physical activities that were once a regular part of life, such as walking a mile or dancing for the duration of one song, can feel especially discouraging.

For patients in their 60s, there are some activities—like jogging—that aren’t especially popular. Even among individuals without CLBP, only 50% of respondents in their 60s reported the ability to jog easily. However, for patients suffering with CLBP, this number plummets to only 13%.

80% of people in their 70s without CLBP are able to easily go up and down the stairs. But the experience may be significantly more challenging for CLBP patients of the same range, as fewer than half of those with CLBP were able to say the same.
Getting up from the floor is another activity that impacts CLBP sufferers much more than their peers who don’t experience chronic pain. While 66% of 70-somethings without CLBP reported ease in getting up or down from the floor, only 28% of those with CLBP were able to say the same.
If you think lumbar spinal stenosis could be causing a patient’s low back pain, and common conservative treatment options such as physical therapy, pain medication, and epidural steroid injections (ESIs) are no longer providing adequate relief, it may be time to move to mild®.
The mild® Procedure, or minimally invasive lumbar decompression, is considered a gold standard of care among treatments for lumbar spinal stenosis. By addressing the root cause of pain, the enlarged ligament, mild® has helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief.

Due to its minimally invasive nature and long-lasting durability, many interventional pain management physicians are making the move to mild® as an alternative to epidural steroid injections (ESIs), which may only work short-term and may require repeat injections to maintain relief.
More invasive courses of treatment can include procedures such as spacer implants or open surgery, though nearly 80% of CLBP sufferers have concerns about undergoing surgery.
For patients experiencing chronic low back pain, it’s never too early to act. Without addressing the root cause of pain—such as the enlarged ligament in cases of LSS—patients can often go years without finding relief.
The Know Your Back Story campaign, a national public health awareness campaign, educates and encourages millions of people with CLBP to learn more about their “back story” and encourages providers to educate patients about LSS and the enlarged ligament that may be the source of this pain.
If your patients are seeking answers for chronic low back pain, they may benefit from the mild® Procedure as a first course of treatment. By referring patients to a local interventional pain management physician, you can help get them on the path to lasting relief.
Access more resources about the Know Your Back Story Campaign and the Mobility Matters Poll
As an Advanced Practice Provider (APP), you are an integral part in helping patients with lumbar spinal stenosis (LSS) get on the path to lasting relief.
In this webinar workshop, led by our panel of mild® experts, APPs Ashley Comer, NP, Marie Zambelli, NP, Kelsey Kimball, PA, Lauren Cote, NP, Patrick McGinn, PA, Kristen Klein, NP, discuss how patient education and proper outcomes assessment play an important role in optimizing patient outcomes after the mild® Procedure.
Access the webinar here:
Looking for more info on mild® patient identification criteria?
Check out our blog: Identifying & Educating mild® Patients – APP Guidance
Sign up to stay informed and receive the latest updates!
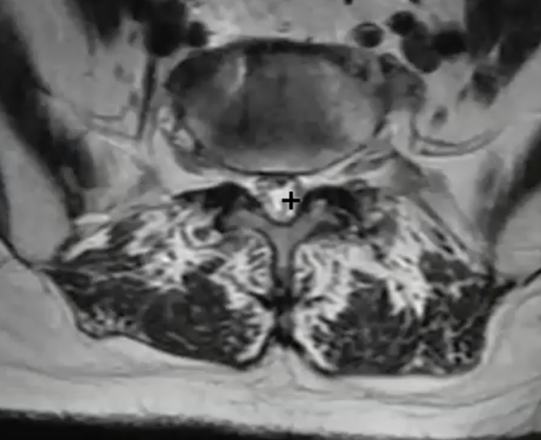
Sign Up NowAccording to our Advanced Practice Provider (APP) Advisory Board, imaging review, a key aspect of mild® patient candidate identification, is often not included in initial schooling. To help APPs learn the basics of image review, become more familiar with identifying anatomical landmarks, and understand how to confirm if a patient is a candidate for the mild® Procedure, we asked James Lynch—an APP with the Pain Consultants of San Diego—to walk us through his tips and techniques for magnetic resonance imaging (MRI) review. In the following article, he shares pearls for becoming confident in imaging review and provides a series of videos so you can follow his step-by-step approach to determine if patients with lumbar spinal stenosis (LSS) should make the move to mild®.
As an APP in an Interventional Pain Medicine practice that offers the mild® Procedure, reviewing MRI images to determine the presence of hypertrophic ligamentum flavum (HLF) is a critical aspect of my role. Prior to joining this practice, I had very little experience reviewing MRI images. It was not part of the core curriculum while training to become an APP, and it was not an area that I felt very confident in. I’ve become more familiar and proficient with imaging review; however, I can say that it’s much more straightforward than it may initially seem. Through hands-on experience, by sharing clinical pearls among peers, and by watching step-by-step videos like those included in this article, I became competent, comfortable, and confident performing image reviews to identify mild® patient candidates—and I know other APPs can too.
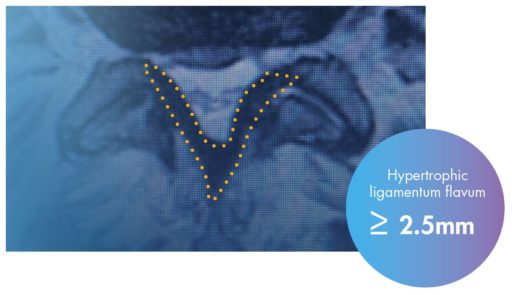
We know that up to 85% of spinal canal narrowing is caused by thickened ligament. When we see patients with symptomatic LSS, if HLF is present, we will likely advance to mild® to provide patients long-term relief using a therapy that has a safety profile equivalent to an epidural steroid injection (ESI), but with lasting results. Being able to review a basic MRI empowers me to identify patients who may benefit from the mild® Procedure and confidently present my recommendations to them. This confidence helps build trust between me and my patients, and makes them feel more comfortable and assured prior to scheduling their mild® Procedure. Having more patients move to mild® means that I’m giving my patients a chance to achieve clinically meaningful, statistically significant improvements in mobility, Oswestry Disability Index (ODI), and pain reduction on the Numeric Pain Rating Scale (NPRS). It’s also incredibly rewarding to hear patients tell me about what they’re able to do now that they can walk further and do more activities than they could before.
LSS is highly recognizable by the signs and symptoms patients commonly exhibit, including pain, numbness, or heaviness when standing or walking, and finding relief by sitting, bending forward, or sleeping curled in the fetal position. When we see these signs in our patients, we’ll order an MRI to confirm the diagnosis and determine whether the patient is a good candidate for the mild® Procedure.
When we request an MRI, we’ll get a report and the imaging back for that patient. During my review of the report, I look line-by-line, specifically confirming whether the report notes central canal stenosis. It is also helpful to make note of other contributors to central canal stenosis (such as enlarged facets, disc bulge, etc.) in order to properly prepare a patient for potential follow-up expectations.

Tip: As you gain comfort with image review, practice reviewing the MRI first and report second to confirm their diagnoses.
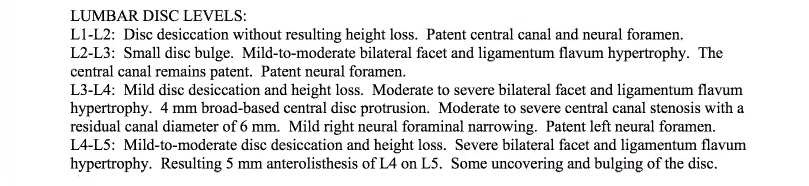
In the example shown here, I would note the following:

Reminder: You can also request that the radiology report include a measurement of the HLF, which can make it easier to review.
Because I have confirmed the presence of central canal stenosis in the report, I’ll then review the imaging to determine whether the patient is a candidate for the mild® Procedure. You can also take the reverse approach and review the imaging first, and then use the radiology report as a confirmation of your own findings.
A note on software: While the specific software demonstrated in this blog is Ambra Health, much of the imaging software used today is similar in function and review procedures. Whether you’re using Ambra Health, Sharp, or another software option, the tips and tricks demonstrated in this blog should be consistent, regardless of the software you’re using.
In pulling up the images, I typically begin setting up the images to facilitate a clear and efficient review process. Begin by adjusting the layout of the software to show 2 images at the same time.
On the left-hand side, we will show the sagittal view, or vertical cross-section of the patient. On the right-hand side, the axial view, or horizontal cross-section of the patient, will be displayed.
Press the “Link” command in the system software to correlate the images together and select the STIR images (T2 weighted images).

Tip: The reason I use the T2 image is because the cerebral spinal fluid actually brightens up, making it a lot easier to assess the spinal canal.
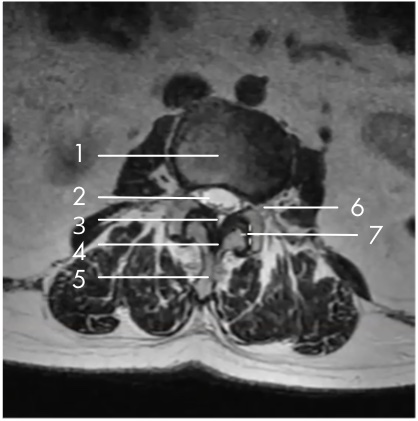

My specific area of interest in evaluating the mild® patient candidate is the small black area, which is the ligamentum flavum, highlighted in the image here.
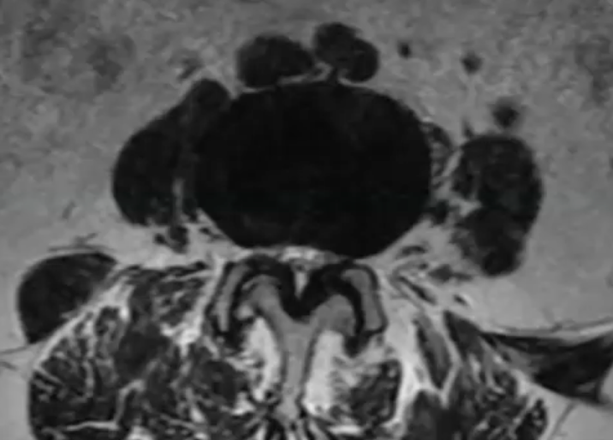
In the small white area, we can see the central canal where the nerves are housed. In this image, we can see that the canal is very small, with very little white showing. This is consistent with central canal stenosis, and in this case, we can see clearly that the hypertrophic ligamentum flavum is compressing the nerves.
By moving our image up to L2-L3, we can see an excellent comparison of the healthy central canal. The large white area shows that at this level, the thin black ligament is not compressing the nerves.
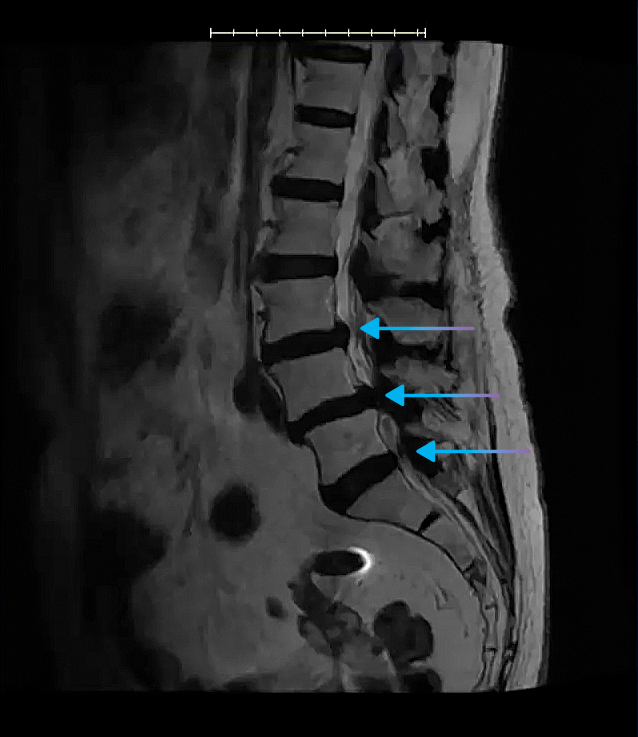
In the sagittal view, you’ll be able to see clearly where the spinal canal narrows, and this is helpful in identifying all levels where the central canal is stenosed.
We can also see here that the patient has a disc bulge, indicative of multi-factorial central canal stenosis.
It’s important to remember that comorbidities are common among LSS patients—in fact, a Level-1 clinical study of mild® patients demonstrated that just 5% of patients presented with central canal stenosis only. The presence of comorbidities, such as foraminal narrowing, lateral recess narrowing, or facet hypertrophy DO NOT RULE OUT patients as mild® Procedure candidates. Indeed, the same clinical study found that the majority of patients with comorbidities achieved an ODI improvement of ≥10 points at 2-year follow-up.
Using the length tool in the software, I can draw a line across the ligament (the dark area indicated in the image below) to obtain the ligament measurement.
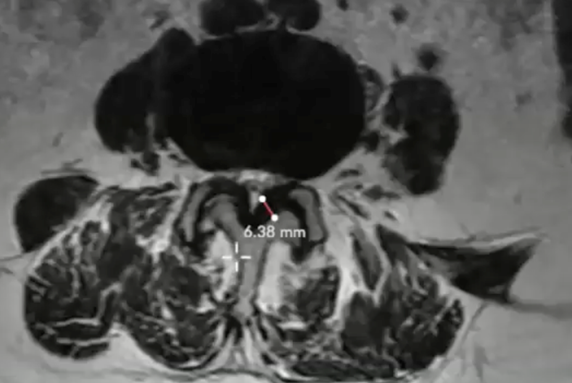
Here, the measurement clearly shows an HLF of 6.38 mm. I will then repeat this measurement process at each of the levels that are affected by central stenosis (per the report, and as seen in the sagittal view).

Tip: As a reminder, any patients with HLF ≥2.5 mm may be considered a candidate for the mild® Procedure.
Once you become familiar with imaging review, you’ll develop your own tips and tricks that make the process easier and more efficient for you. Here are a few things that I suggest that can help when you’re just getting started:
In this video, you can see an end-to-end example of the imaging review for an ideal mild® case. In under 5 minutes, you can see how I:
When a patient can’t have an MRI, we will instead send them in for a computed tomography (CT), ideally with a myelogram. A myelogram will highlight these relevant anatomical structures, so you can see the ligament and determine the patient’s candidacy. Even if a myelogram is not an option, be sure to indicate a primary diagnosis for lumbar stenosis when you order the CT, and the radiologist will then assess that patient for lumbar stenosis and HLF.
When patients are in the office, I’ll often bring my laptop into the exam room and show them their imaging on screen. Being able to see their own anatomy, and specifically the hypertrophic ligament pressing on the nerves, is incredibly helpful to demonstrate this root cause of their LSS.
Then, I can also use the imaging to clearly point out how mild® addresses a major root cause of LSS by removing excess ligament tissue and leaving no implants behind. I’ll also show them where the nerves are being compressed and educate them about how mild® restores space in the spinal canal, which reduces the compression of the nerves. Most patients understand how the mild® Procedure works much more easily when they can see the images themselves, and it also helps them realize how the mild® Procedure can provide long-term relief and restore mobility.
When I first started with imaging review, I was much less comfortable and confident than I am today. Knowing that our practice is committed to helping more patients move to mild®, I recognized that becoming comfortable with imaging review was a critical aspect of my role. Even though MRI review was not something included in my initial APP education, I realized that becoming proficient gave me an opportunity to bring additional value to our patients and practice.
The best way I found to get comfortable with imaging review was to dive in and review previous cases so I could become familiar with the anatomy and structures. Beyond hands-on experience, there are resources that offer additional support, including:
With additional practice and experience, you’ll quickly become much more comfortable with imaging review. You’ll also notice how many of your patients with LSS have HLF and are candidates for the mild® Procedure. By putting more patients on the path to lasting relief with mild®, you’ll get to see first-hand how regaining mobility can be a life-changing improvement for the patients in your care.
Advanced Practice Providers (APPs) play a vital role in helping patients understand their lumbar spinal stenosis (LSS) diagnosis and treatment recommendations. By developing strong provider-patient communication, you’re taking the first step towards achieving positive outcomes and enhancing the patient experience.
Why is patient education so important?
Based on the data above, it is clear that patients over 65 years of age–the group most likely to suffer from LSS–may need more support to understand their condition and treatment plan. With the recognition that both lumbar spinal stenosis and poor health literacy can increase your patients’ susceptibility to poor physical functioning, pain, and limitations in activities of daily living, APPs should feel especially empowered to engage patients. This includes helpful education and dialogue that supports their understanding and helps them feel more comfortable taking the next step on their path to lasting relief.
In the following article, you will find step-by-step guidance and pragmatic suggestions that you can start using today, to help you ensure that your patients leave their consultation feeling confident and excited about their opportunity to make the move to mild®.
Watch: See APP Ashley Comer’s complete talk track for presenting mild® to her LSS patients.
Use the mild® patient brochure as a tool and follow these simple steps to help your patients better understand their lumbar spinal stenosis diagnosis and the benefits of the mild® Procedure.
![]()
Instead of using complex medical terms or acronyms, simplify your explanation with common words, phrases, and analogies to help patients understand their diagnosis and treatment options.
According to the CDC, nearly 9 out of 10 adults struggle to understand and use personal health information when it’s filled with unfamiliar or complex terms. (Source)
On the first page of the mild® patient brochure, you’ll find helpful illustrations that demonstrate the anatomical changes associated with LSS and the symptoms patients typically experience. During your patient consultation, be sure to highlight:
![]()
Many APPs and physicians use common, real-life analogies to help patients identify and understand their LSS symptoms. A common analogy that many patients may relate to is the “shopping cart syndrome.” Explaining that patients with lumbar spinal stenosis often feel relief when bending over a shopping cart (because it reduces pressure on the compressed nerves) can help patients recognize how this condition impacts their daily life.
Once you’ve established the common signs and symptoms of LSS, demonstrate what the MRI shows for that specific patient. Turn to the last page of the mild® patient brochure, where you can use the diagrams provided. Drawing directly on the patient brochure, indicate the following:
Watch: See how APP Ashley Comer uses the illustrations in the mild® patient brochure to demonstrate her patients’ specific areas of stenosis.
You can also accompany the spinal illustrations in the mild® patient brochure with an added tool, such as a spine model or the patient’s MRI to reinforce the anatomical positioning of the problem or validate the diagnosis, respectively.
Once patients fully understand their condition, walk them through all of the reasons why you recommend they make the move to mild®. If you turn back to the beginning of the brochure (or access the same information in the mild® patient flip chart) and review the remaining pages, you can quickly cover the advantages of mild® relative to other treatment options, and prepare your patients for what to expect during and after their mild® Procedure.
Because epidural steroid injections (ESIs) were historically the standard of care for lumbar spinal stenosis patients, your patient may be expecting you to recommend another injection. You can explain that the data shows that there is no benefit to giving more than one ESI before mild®, and that giving more than one ESI delays the patient from receiving the longer-lasting, more effective mild® Procedure.

![]()
Every year, thousands of lumbar spinal stenosis patients are able to stand longer and walk farther with less pain thanks to the mild® Procedure, but those results aren’t achieved overnight. Improvements in patient functionality are typically achieved over time, with patients gradually increasing standing time and walking distance. If you set expectations in advance, patients may be more excited and satisfied to see their own functional improvements over time.
LSS patients rely on APPs as critical members of their care team. Across the patient journey from diagnosing your patients’ LSS to finding relief with the mild® Procedure, APPs are key in supporting patients, helping them understand their condition, and feeling confident about their decision to make the move to mild®.
At Vertos, we recognize and support the role of APPs and are committed to providing education and resources that help you put more LSS patients on the path to lasting relief.
Don’t miss out on the latest and greatest tips and tools from Vertos.
Interventional Pain Management is a fast-growing specialty. As new lumbar spinal stenosis (LSS) procedures become available, practices are evolving the way they collaborate and work together to optimize patient care. The mild® Procedure’s patient selection process is quite simple, but requires imaging review, which is often not a part of Advanced Practice Providers’ (APP) traditional education.
The Vertos APP Advisory Board has emphasized the need for educational tools for APPs who would like to develop their image review skillset. Two of the esteemed Vertos APP Board Members, James Lynch, PA and Kelsey Kimball, PA, partnered with their physicians Dr. Michael Verdolin and Dr. Ajay Antony to provide an interactive workshop focused on enhancing imaging review skillsets. View the interactive workshop where they cover imaging basics, navigating software, measuring the ligament, and more!
Looking for more info on mild® patient identification criteria? Check out our blog: Identifying & Educating mild® Patients – APP Guidance.
Also, be sure to connect with us to stay informed of upcoming APP-specific educational and peer engagement opportunities. Sign up and receive the latest updates!
Sign Up NowInterventional Pain Management is a fast-growing specialty. As new lumbar spinal stenosis (LSS) procedures become available, practices are evolving the way they collaborate and work together to optimize patient care. The mild® Procedure’s patient selection process is quite simple, but requires imaging review, which is often not a part of Advanced Practice Providers’ (APP) traditional education.
Although image review can be intimidating, APPs report that the learning curve is relatively short and there are resources available to help you get started. Below are some tips from mild® APPs on how they quickly established comfort with imaging review in their practice, allowing them to “look for the ligament,” identify hypertrophic ligamentum flavum (HLF), and educate mild® patients independently.

In a prior CME webinar hosted by the American Society of Pain & Neuroscience (ASPN), moderators Timothy Deer, MD; Dawood Sayed, MD and faculty members Navdeep Jassal, MD; Eugene Paik, MD; Ashley Comer, NP-C; Christine Christensen, APRN; and Zohra Hussaini, MSN, FNP-BC, MBA, APRN discussed how physicians and APPs can match more patients with the right treatments sooner by working together.
Visit ASPN’s websiteLooking for more info on mild® patient identification criteria? Check out our blog: Identifying & Educating mild® Patients – APP Guidance. Interested in APP-focused education and events? Sign up to stay informed and receive the latest updates!
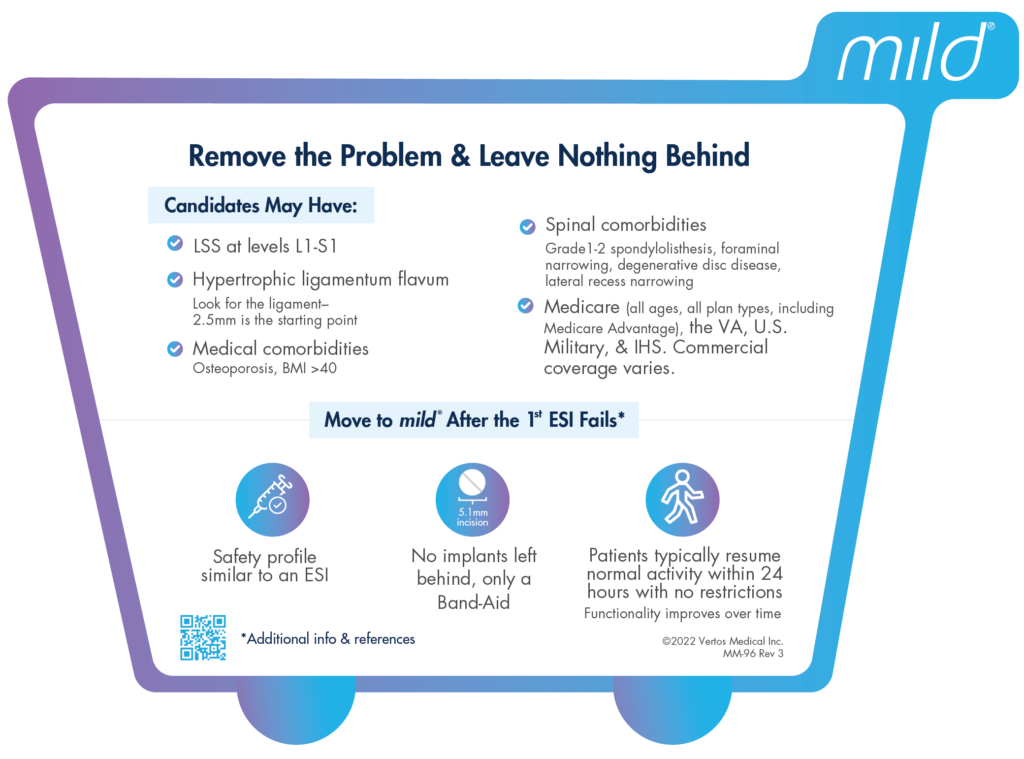
Sign Up NowInjections falling short? Advanced IPM practices are moving beyond epidural steroid injections (ESIs) to offer the gold standard of care for lumbar spinal stenosis (LSS) patients. Review the new data where study researchers compared the medical records of participants who had received either just one or no steroid injection prior to the mild® Procedure, to participants who received two or more epidural steroid injections prior to mild®. Similar outcomes in both treatment groups in this study proved that giving more than one ESI prior to the mild® Procedure did not improve how well patients did and may have delayed patient care. Based on the results of the study, it is recommended that the standard treatment process for LSS patients be changed to give the mild® Procedure either as soon as LSS is diagnosed or after the failure of the first ESI.
Congratulations to authors and mild® physicians Peter Pryzbylkowski, Anjum Bux, Kailash Chandwani, Vishal Khemlani, Shawn Puri, Jason Rosenberg and Harry Sukumaran for the first ever plain language article to be published in Pain Management!
View the original article and share the plain language version with your community.



If your lumbar spinal stenosis (LSS) treatment algorithm relies on serial epidural steroid injections (ESIs) to relieve chronic lower back and leg pain associated with neurogenic claudication, data supports a different approach—performing the mild® Procedure immediately upon diagnosis of LSS or moving to mild® after the first ESI fails may help your patients avoid “ESI Exhaustion.”
We already know that epidurals are not capable of “curing” neurogenic claudication, a major root cause of lumbar spinal stenosis which is present in 94% of patients. The steroids in the injection are believed to reduce inflammation to relieve pain; however, injections are only treating the symptoms of LSS. For long lasting relief, debulking the ligament is required. Injections results typically last less than six months. To provide ongoing relief, patients often require 2-3 injections on average per year.


Due to the temporary nature of epidural steroid injection relief, and the requirement for repeat injections, many practices encounter patients with what is increasingly becoming known as “ESI Exhaustion.” ESI Exhaustion can be spotted in patients at any stage of LSS treatment or stenosis severity. Once you start recognizing the signs of ESI Exhaustion in your lumbar spinal stenosis patients, you’ll see why so many leading clinicians are moving to mild® earlier in their treatment algorithm.
When patients experience short-term relief for a condition as challenging as LSS, it can be easy for them to become frustrated and lose hope. Patients can become tired from needing to return for repeat injections. Other patients may start to feel hopeless if the injection is not effective or if it is only effective for a very short time. It’s important to remember that LSS patients often experience debilitating pain and loss of mobility that can have a devastating impact on their quality of life.
To help your patients remain optimistic and aligned to your treatment plan, educate your new and existing LSS patients about your treatment options early. Make sure they know that there is a procedure that offers the safety equivalence of an ESI, but with lasting results. If you are starting their treatment plan with a single epidural, inform them about the mild® Procedure during that first visit, so they know that if the ESI is not effective, there are other options that can help restore mobility by addressing a major root cause of LSS.

One of the more common questions patients have about a steroid injection is “how long will the results last?” Unfortunately, with ESIs, efficacy can vary by patient, and it can be difficult to predict the degree of relief or durability of effect for each. While studies have shown pain relief for up to six months in some lumbar spinal stenosis patients receiving steroid injections, other studies have demonstrated limited effectiveness.

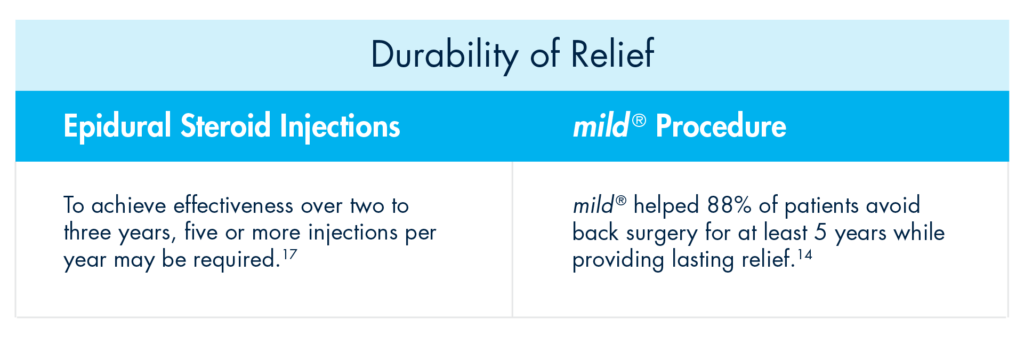
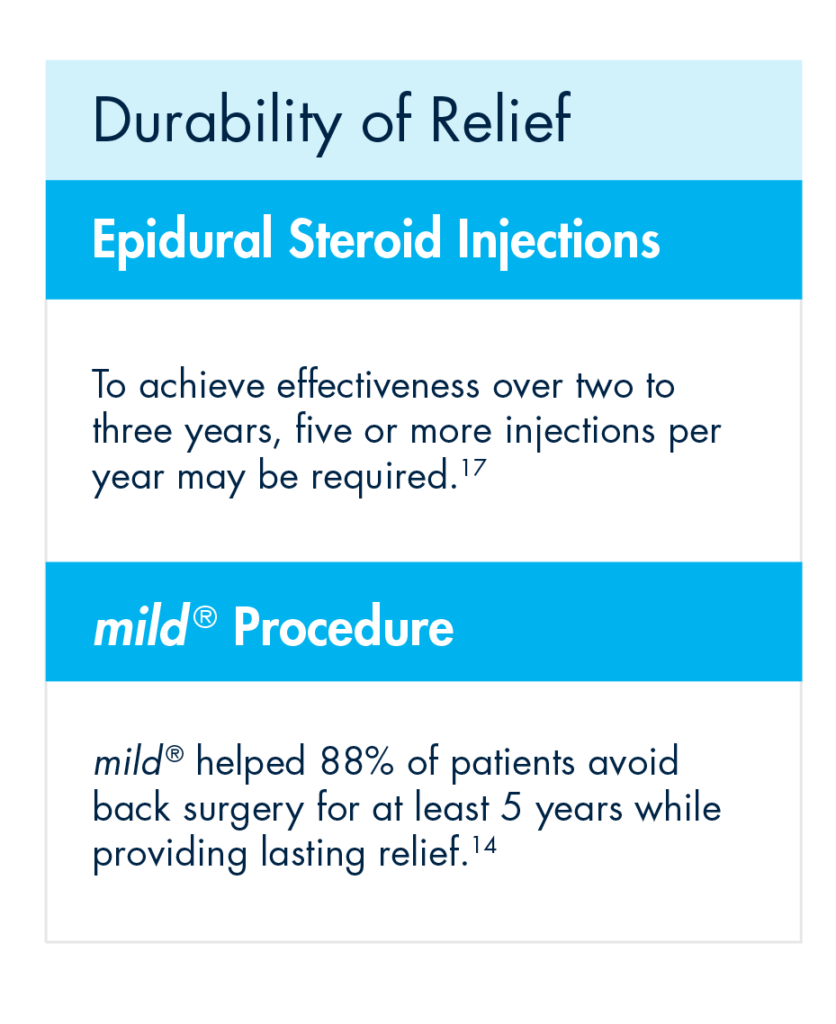
Even more vexing for some patients is that the durability of effect of an initial ESI may not be experienced with subsequent injections. To achieve effectiveness over two to three years, five or more injections per year may be required.
Rather than offering patients a series of injection after injection with short-term results, move to mild® after the first ESI fails. The mild® Procedure offers a clinically proven safety profile equivalent to ESIs, but with lasting results. A 5-year study completed by the Cleveland Clinic showed that mild® helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief.
If patients are dissatisfied with their results and feel they’ve run out of options in your practice, they may start to search for another solution. By offering mild® as an early intervention, you can avoid losing patients and actually increase productivity in your practice. Upon diagnosis of LSS, inform patients that you offer mild®, a minimally invasive treatment option that offers durable relief.
If you have already treated a patient with an ESI and it failed, or the patient received an injection in another practice, there is no reason to continue to offer another injection. Most patients I’ve seen are excited to learn that there is another option. Moving to mild® gives them new hope in finding lasting relief.
While “ESI Exhaustion” is highly common among LSS patients, it is also completely avoidable. Recognizing that serial injections are often the standard of care when conservative care methods like exercise and physical therapy have failed to provide relief, we published a study in Pain Management that evaluated whether LSS patients benefit from multiple ESIs prior to mild®.
The article, ‘Minimally invasive direct decompression for lumbar spinal stenosis: impact of multiple prior epidural steroid injections’ compares outcomes between 145 patients receiving either 0/1 injections or 2+ injections at 6 centers in the United States. In reviewing results between the two groups, we concluded that there is no benefit to performing multiple epidural steroid injections before the mild® Procedure and that doing so delays the patient from receiving a longer-lasting, more effective mild® treatment.
Based on this study and other favorable data, we recommend performing the mild® Procedure for lumbar spinal stenosis patients immediately upon diagnosis of neurogenic claudication with hypertrophic ligamentum flavum, or after the first ESI fails.
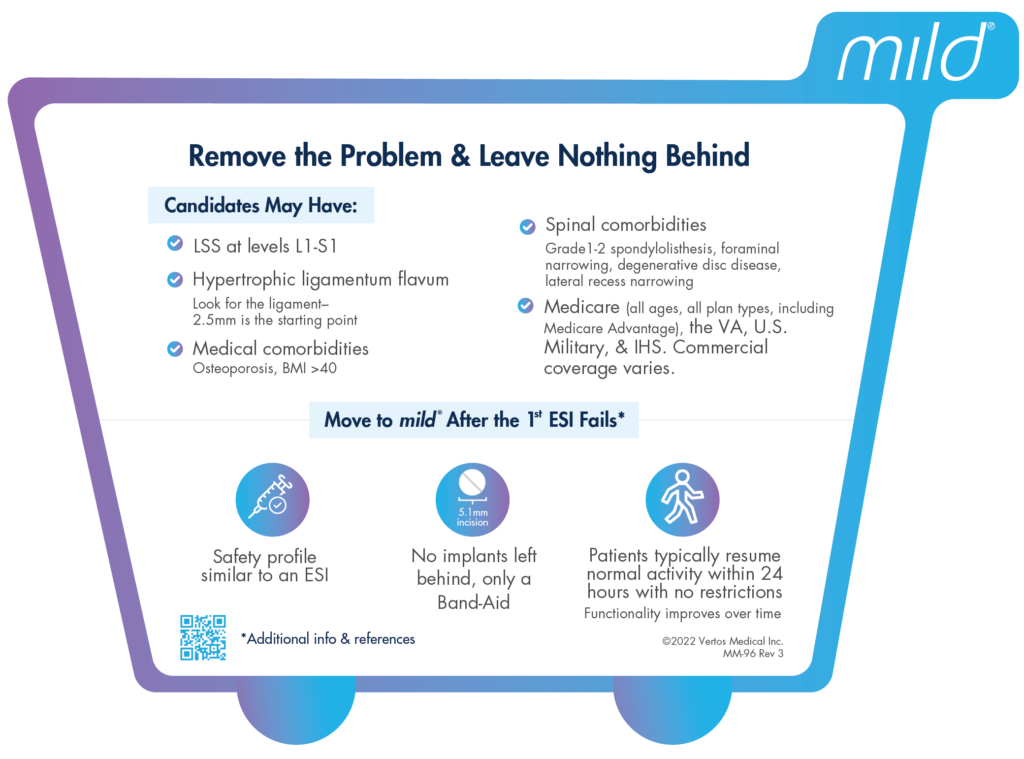
Does your practice offer the mild® Procedure? Do you manage patient identification and education? Follow these 3 steps to optimize your practice routine:
Shopping Cart Syndrome – lumbar spinal stenosis (LSS) with neurogenic claudication (NC). These patients will often be the first ones to find chairs in your waiting room or use the walking aids, such as a shopping cart, to establish a flexed position. The flexed posture is a common sign of NC because it opens up the spinal canal to alleviate the pressure on the central canal to avoid pain that comes with being straight, upright, or mobile.
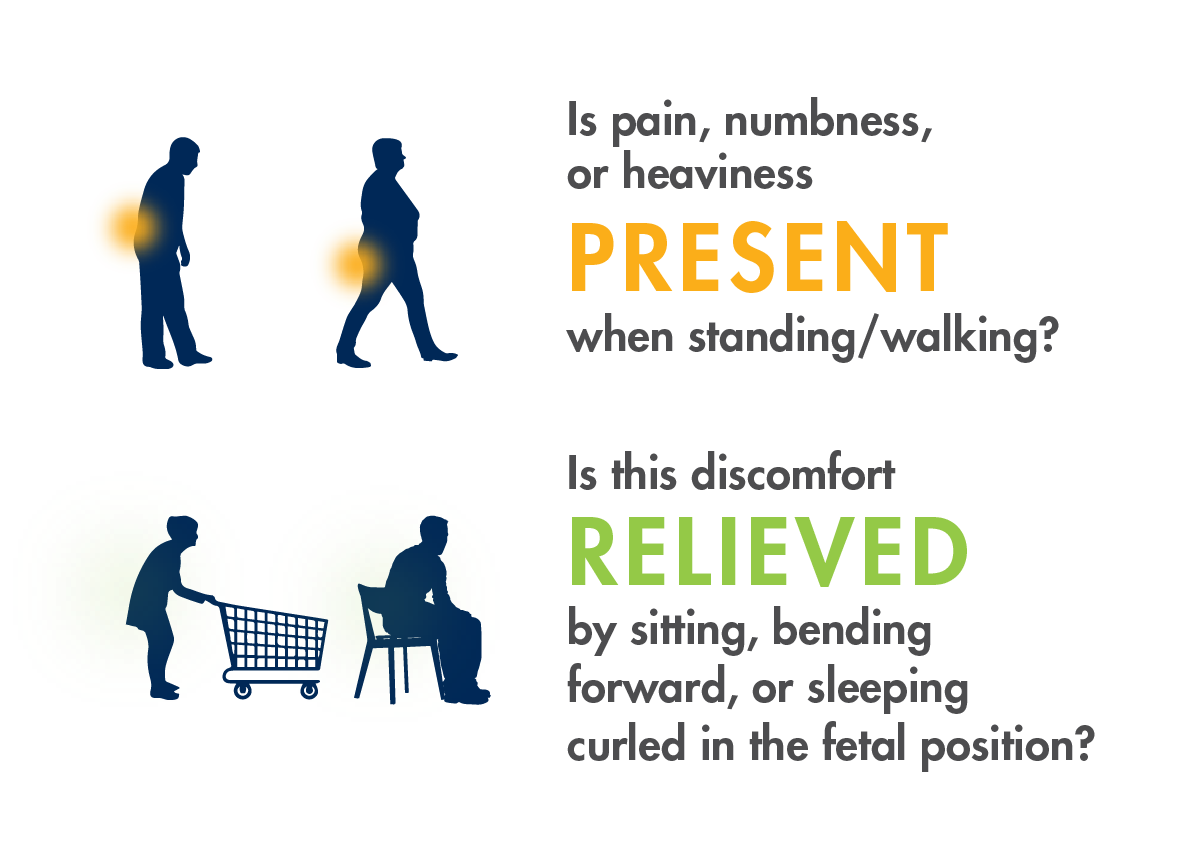
Ask patients the following questions to better understand how LSS with neurogenic claudication is limiting their mobility and when they experience symptom onset. Patients commonly report pain, so it is essential to talk about their functional limitations (eg, desire to walk the dog, get the mail, play with their grandchildren, etc.).
Consider incorporating these questions into your EMR or intake process so patients are routinely screened for neurogenic claudication.
Ask patients the following questions to better understand how LSS with neurogenic claudication is limiting their mobility and when they experience symptom onset. Patients commonly report pain, so it is essential to talk about their functional limitations (eg, desire to walk the dog, get the mail, play with their grandchildren, etc.).
Consider incorporating these questions into your EMR or intake process so patients are routinely screened for neurogenic claudication.
Hypertrophic ligamentum flavum (HLF) contributes up to 85% of spinal canal narrowing
mild® is covered nationwide by Medicare and Medicare Advantage. Commercial coverage and other plans vary.
![]()
mild® helps patients stand longer and walk farther with less pain.
If you would like a mild® Quick Reference Card for your office or to learn more about APP-specific educational opportunities, please contact us and let us know what you need.
Benyamin RM, Staats PS, MiDAS ENCORE Investigators. mild® is an effective treatment for lumbar spinal stenosis with neurogenic claudication: MiDAS ENCORE Randomized Controlled Trial. Pain Physician. 2016;19(4):229-242.
Mekhail N, Costandi S, Abraham B, Samuel SW. Functional and patient-reported outcomes in symptomatic lumbar spinal stenosis following percutaneous decompression. Pain Pract. 2012;12(6):417-425. doi:10.1111/j.1533-2500.2012.00565.x.
2012 data from Health Market Sciences report for Vertos Medical 2013.
Data on file with Vertos Medical.
Staats PS, Chafin TB, Golvac S, et al. Long-term safety and efficacy of minimally invasive lumbar decompression procedure for the treatment of lumbar spinal stenosis with neurogenic claudication: 2-year results of MiDAS ENCORE. Reg Anesth Pain Med. 2018;43:789-794. doi:10.1097/AAP.0000000000000868.
Based on mild® Procedure data collected in all clinical studies. Major complications are defined as dural tear and blood loss requiring transfusion.
MiDAS ENCORE responder data. On file with Vertos Medical.
Jain S, Deer TR, Sayed D, et al. Minimally invasive lumbar decompression: a review of indications, techniques, efficacy and safety. Pain Manag. 2020;10(5). https://doi.org/10.2217/pmt-2020-0037. Accessed June 1, 2020.
Deer TR, Grider JS, Pope JE, et al. The MIST Guidelines: the Lumbar Spinal Stenosis Consensus Group guidelines for minimally invasive spine treatment. Pain Pract. 2019;19(3)250-274. doi:10.1111/papr.12744.
Hansson T, Suzuki N, Hebelka H, Gaulitz A. The narrowing of the lumbar spinal canal during loaded MRI: the effects of the disc and ligamentum flavum. Eur Spine J. 2009;18(5):679-686. doi:10.1007/s00586-009-0919-7.
Treatment options shown are commonly offered once conservative therapies (e.g., physical therapy, pain medications, chiropractic) are not providing adequate relief. This is not intended to be a complete list of all treatments available. Doctors typically recommend treatments based on their safety profile, typically prioritizing low risk/less aggressive procedures before higher risk/more aggressive procedures, but will determine which treatments are appropriate for their patients.
The mild® Procedure is a minimally invasive treatment for lumbar spinal stenosis. As with most surgical procedures, serious adverse events, some of which can be fatal, can occur, including heart attack, cardiac arrest (heart stops beating), stroke, and embolism (blood or fat that migrates to the lungs or heart). Other risks include infection and bleeding, spinal cord and nerve injury that can, in rare instances, cause paralysis. This procedure is not for everyone. Physicians should discuss potential risks with patients. For complete information regarding indications for use, warnings, precautions, and methods of use, please reference the devices’ Instructions for Use.
Patient stories on this website reflect the results experienced by individuals who have undergone the mild® Procedure. Patients are not compensated for their testimonial. The mild® Procedure is intended to treat lumbar spinal stenosis (LSS) caused by ligamentum flavum hypertrophy. Although patients may experience relief from the procedure, individual results may vary. Individuals may have symptoms persist or evolve or other conditions that require ongoing medication or additional treatments. Please consult with your doctor to determine if this procedure is right for you.
Reimbursement, especially coding, is dynamic and changes every year. Laws and regulations involving reimbursement are also complex and change frequently. Providers are responsible for determining medical necessity and reporting the codes that accurately describe the work that is done and the products and procedures that are furnished to patients. For this reason, Vertos Medical strongly recommends that you consult with your payers, your specialty society, or the AMA CPT regarding coding, coverage and payment.
Vertos Medical cannot guarantee coding, coverage, or payment for products or procedures. View our Billing Guide.
Vertos is an equal employment opportunity workplace committed to pursuing and hiring a diverse workforce. We strive to grow our team with highly skilled people who share our culture and values. All qualified applicants will receive consideration for employment without regard to sex, age, color, race, religion, marital status, national origin, ancestry, sexual orientation, gender identity, physical & mental disability, medical condition, genetic information, veteran status, or any other basis protected by federal, state or local law.
Hall S, Bartleson JD, Onofrio BM, Baker HL Jr, Okazaki H, O’Duffy JD. Lumbar spinal stenosis. Clinical features, diagnostic procedures, and results of surgical treatment in 68 patients. Ann Intern Med. 1985;103(2):271-275. doi:10.7326/0003-4819-103-2-271.
Kalichman L, Cole R, Kim DH, et al. Spinal stenosis prevalence & association with symptoms: The Framingham Study. Spine J. 2009;9(7):545-550. doi:10.1016/j.spinee.2009.03.005.
Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998;14(2):148-151. doi:10.1097/00002508-199806000-00010.
Mekhail N, Costandi S, Nageeb G, Ekladios C, Saied O. The durability of minimally invasive lumbar decompression procedure in patients with symptomatic lumbar spinal stenosis: Long-term follow-up [published online ahead of print, 2021 May 4]. Pain Pract. 2021;10.1111/papr.13020. doi:10.1111/papr.13020
Friedly JL, Comstock BA, Turner JA, et al. Long-Term Effects of Repeated Injections of Local Anesthetic With or Without Corticosteroid for Lumbar Spinal Stenosis: A Randomized Trial. Arch Phys Med Rehabil. 2017;98(8):1499-1507.e2. doi:10.1016/j.apmr.2017.02.029
Pope J, Deer TR, Falowski SM. A retrospective, single-center, quantitative analysis of adverse events in patients undergoing spinal stenosis with neurogenic claudication using a novel percutaneous direct lumbar decompression strategy. J Pain Res. 2021;14:1909-1913. doi: 10.2147/JPR.S304997
Pryzbylkowski P, Bux A, Chandwani K, et al. Minimally invasive direct decompression for lumbar spinal stenosis: impact of multiple prior epidural steroid injections [published online ahead of print, 2021 Aug 4]. Pain Manag. 2021;10.2217/pmt-2021-0056. doi:10.2217/pmt-2021-0056
Abstract presented at: American Society of Pain and Neuroscience Annual Conference; July 22-25, 2021; Miami Beach, FL.
Mobility Matters: Low Back Pain in America, Harris Poll Survey, 2022. View data and full summary here.
Deer TR, Grider JS, Pope JE, et al. Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST): Consensus Guidance from the American Society of Pain and Neuroscience (ASPN). J Pain Res. 2022;15:1325-1354. Published 2022 May 5. doi:10.2147/JPR.S355285.