Peter Pryzbylkowski, MD (00:00)
My name is Dr. Peter Pryzbylkowski. I’m a board certified anesthesiologist and board certified interventional pain specialist with the Relievus Pain Management Group, based out of the Philadelphia area. I want to thank Vertos, number one, for getting me involved with this study.
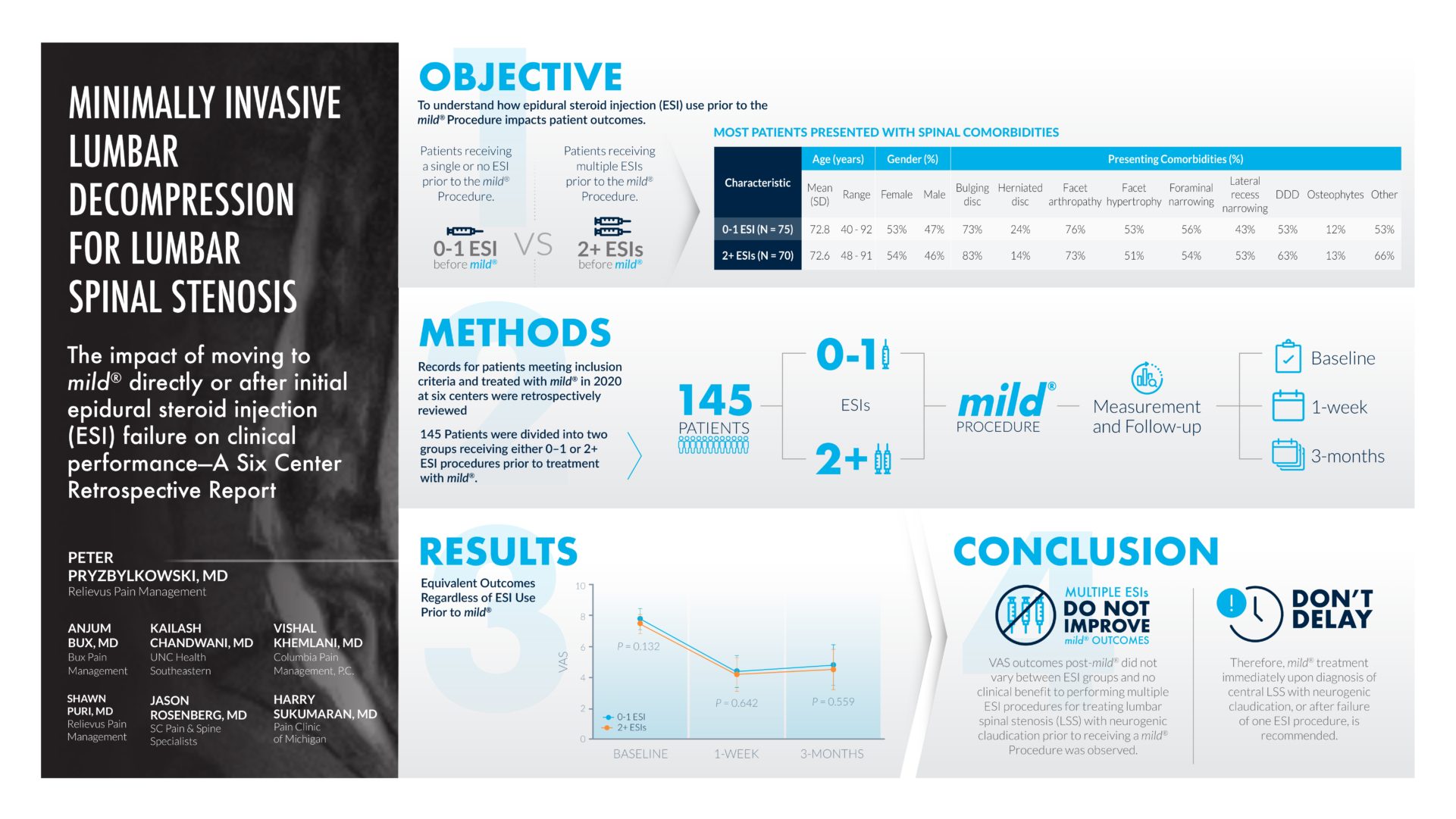
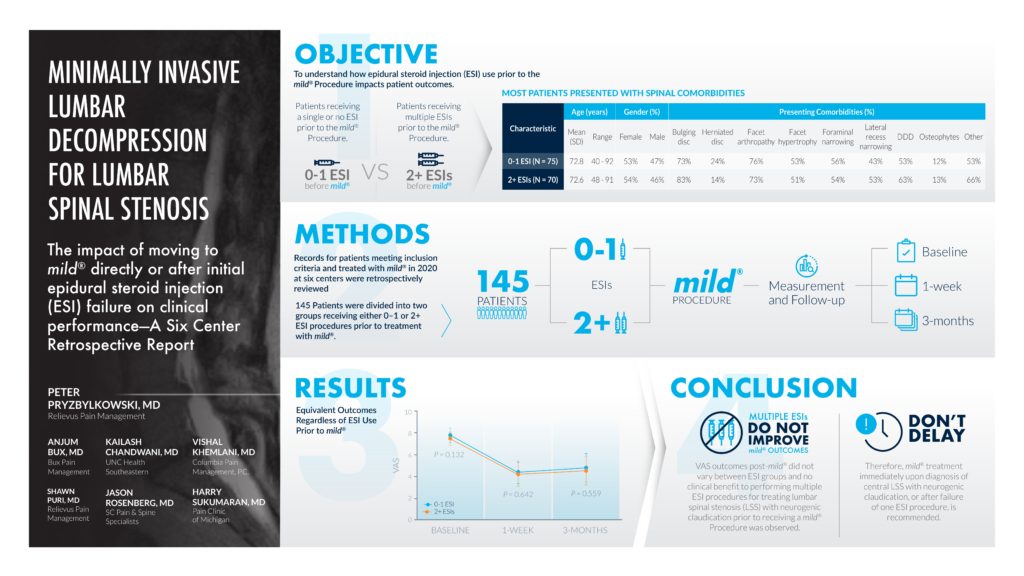
So, the objective of this study was to determine whether or not, no epidurals, one epidural versus a series of epidurals, made any difference in terms of pain relief, pain reduction, post-mild® Procedure. So, this is a nice clinical study because it kind of expands the bandwidth of practices across the country.
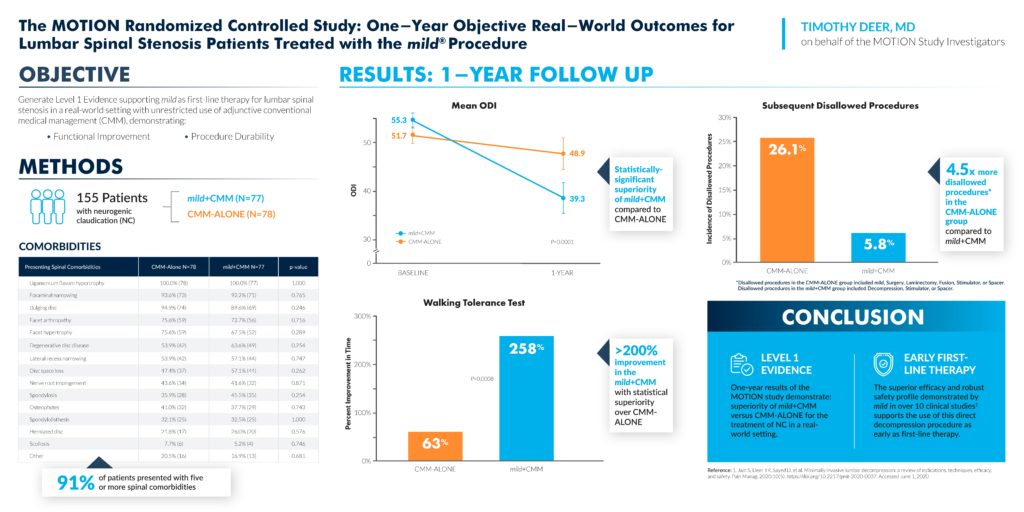
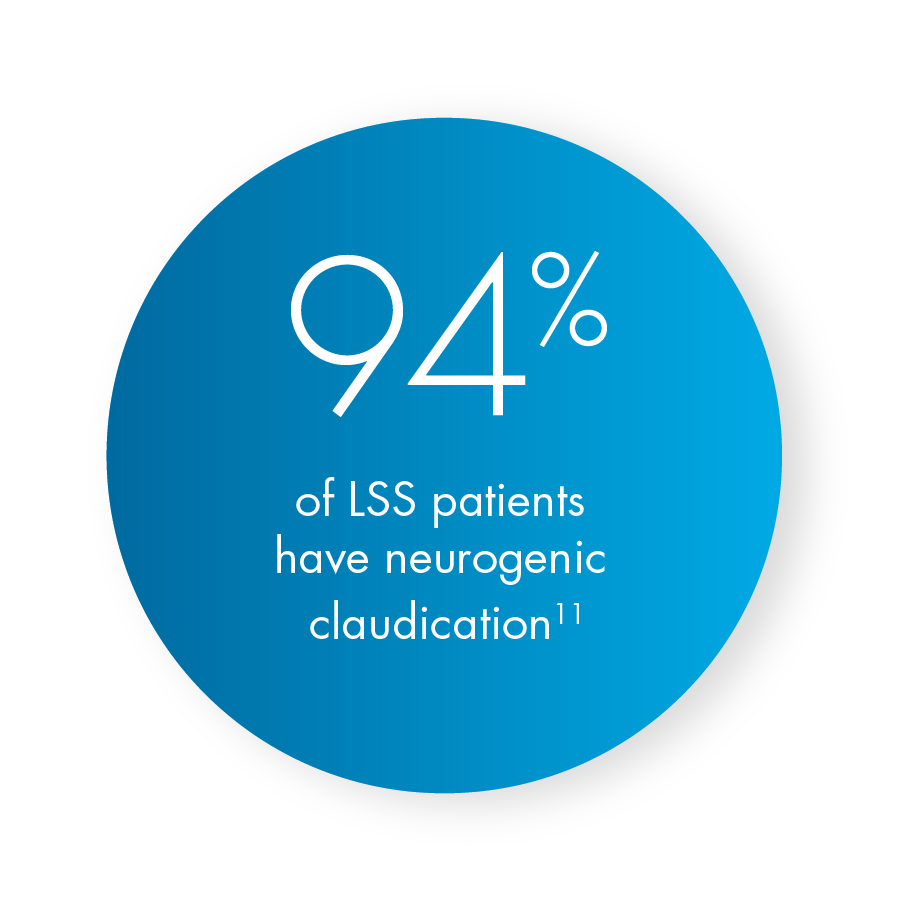
So, we have 6 total centers, 145 patients, that was enrolled in this study. Basically it was a retrospective review of patient charts we all did, and it’s important to notice, specifically under the objective tab, that the comorbid conditions coexisting, with patients with lumbar spinal stenosis with neurogenic claudication, is noted there, so these patients had bulging discs, herniated discs, facet arthropathy, facet hypertrophy, narrowing of the foramen, degenerative disc disease, osteophytes, and other comorbid conditions, so even though these patients had other comorbid conditions that are listed there, these patients still had good clinical and durable clinical results after post decompression procedure.
So, you can see the average ages there, the breakdown of male versus female, and those comorbid conditions I had mentioned before. And the groups we’re looking at, so it’s a group of patients who either had no epidurals or one epidural, versus two or more epidurals. So 145 patients total, were looked at in this retrospective review, and we followed the results, both at the baseline pre-procedure, one week post-operatively, and 3 months after mild® Procedure was performed. And, what you can see in the results section is that multiple epidurals versus no epidurals or one epidural did not make a difference in terms of VAS scores post-mild® Procedure.
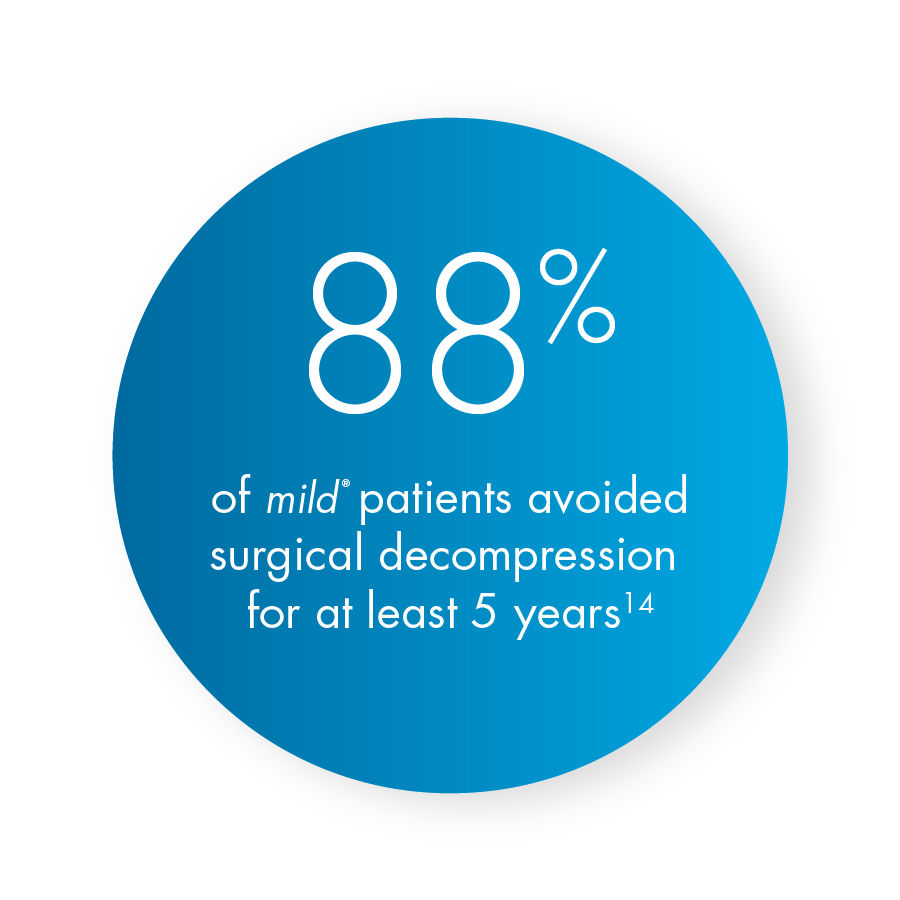
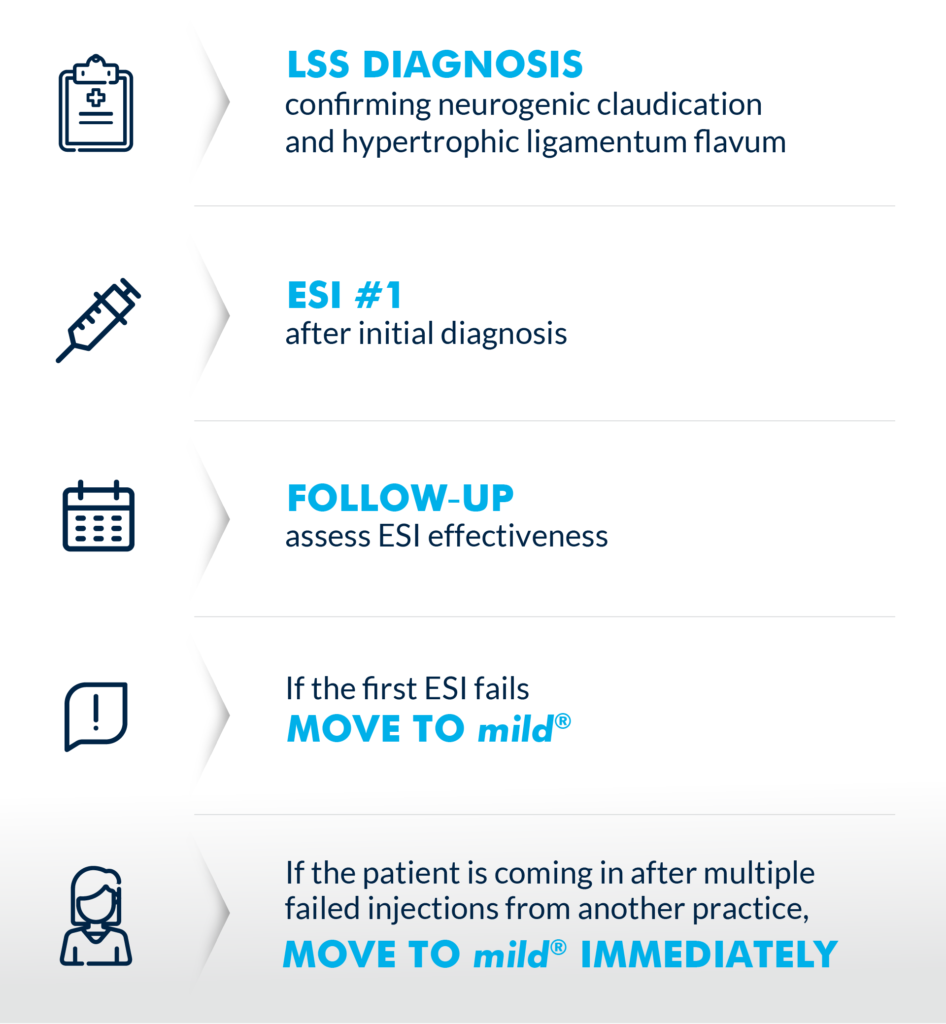
(02:13) So, really what this is telling us as pain providers, is it doesn’t matter if you do no epidurals, one epidural or multiple. It’s not gonna affect your clinical outcome post-mild® Procedure, so the take home message from a retrospective review like this is that really, doing epidurals, a series of epidurals, really, we know as pain doctors, doesn’t really provide long-term clinical benefit, and it’s not gonna affect the outcome post-lumbar decompression. So if you have a patient with lumbar spinal stenosis with neurogenic claudication, they have ligamentum flavum hypertrophy, they’re candidates for the mild® Procedure and it’s important to do the procedure sooner rather than later ’cause all you’re really doing with a series of epidurals is delaying appropriate care, so kind of the message that this has hit home in my own personal practice is, I’ve really been able to go to all my advanced providers and say, “Listen, if we have patients who are kind of stuck in this rut of doing multiple epidurals, epidural, epidural, epidural for their lumbar spinal stenosis, we should really be considering doing the mild® Procedure to help give them good long-term benefit, rather than giving them multiple injections, which increases the risk of infection, increases the risk of an untoward side-effect.” Obviously every time we do a procedure there’s always a risk.
It’s nice to do a procedure that can give them long-term benefit, so if you have patients that have spinal stenosis, it’s just important to keep in mind mild® as a first treatment step rather than treatment that you would consider down the road for patients with spinal stenosis with neurogenic claudication. So I would not delay treating these patients when they come to my clinic. So, I used to do an epidural, 2 epidurals, 3 epidurals, for patients with spinal stenosis with neurogenic claudication. The outcomes really were hit or miss, so for me personally, I’m offering these patients percutaneous decompression in the form of the mild® Procedure a lot sooner than I used to 2-3 years ago. And the data from this retrospective study kind of shows that by doing the procedure sooner rather than later, not delaying care, we can give them good long-term benefit, give them a procedure that’s actually indicated for their pathology and approved for their pathology, rather than delaying care with a series of epidurals.

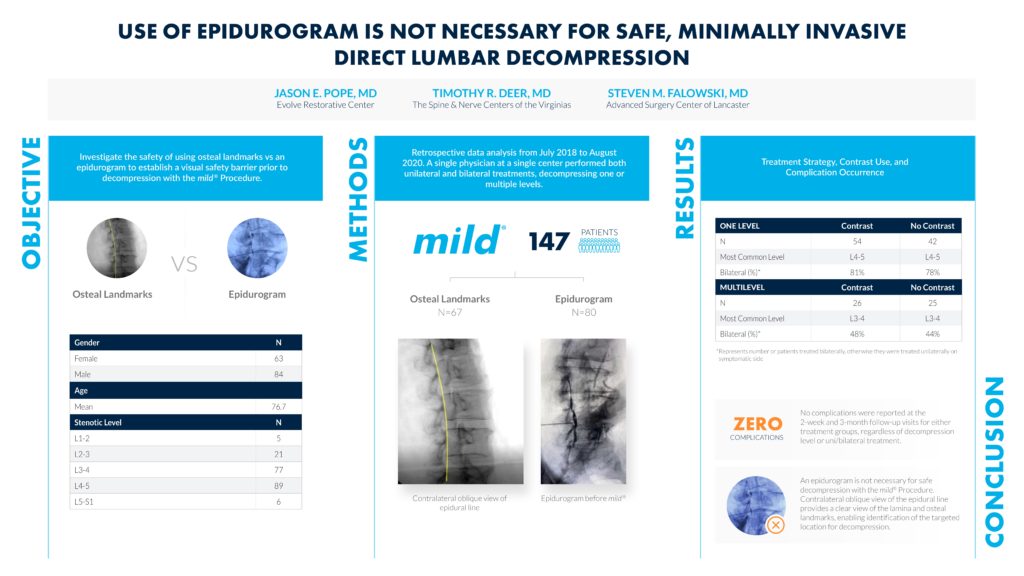


 Jason Pope, MD, is an Interventional Pain Physician trained in Pain Medicine at the Cleveland Clinic with board certifications in Anesthesia and Pain Medicine. He completed an Anesthesiology Residency at Vanderbilt University Medical Center and received his medical degree from the Indiana University School of Medicine. Dr. Pope is the Founder and CEO of Evolve Restorative Center in Northern California and serves as an expert reviewer for the Medical Board of California. Dr. Pope also serves as President Emeritus and Chairman for the
Jason Pope, MD, is an Interventional Pain Physician trained in Pain Medicine at the Cleveland Clinic with board certifications in Anesthesia and Pain Medicine. He completed an Anesthesiology Residency at Vanderbilt University Medical Center and received his medical degree from the Indiana University School of Medicine. Dr. Pope is the Founder and CEO of Evolve Restorative Center in Northern California and serves as an expert reviewer for the Medical Board of California. Dr. Pope also serves as President Emeritus and Chairman for the  Heidi Younan is the Director of Patient Marketing & Practice Integration at Vertos Medical. A critical member of the Vertos team for over a decade, Ms. Younan works with clinicians, APPs, and patients to support the successful integration of the
Heidi Younan is the Director of Patient Marketing & Practice Integration at Vertos Medical. A critical member of the Vertos team for over a decade, Ms. Younan works with clinicians, APPs, and patients to support the successful integration of the